January/February 2019
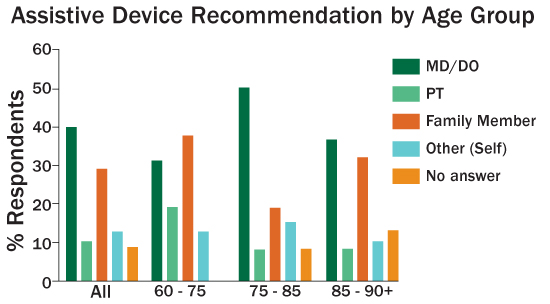
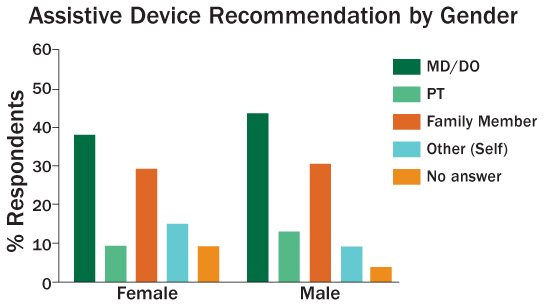
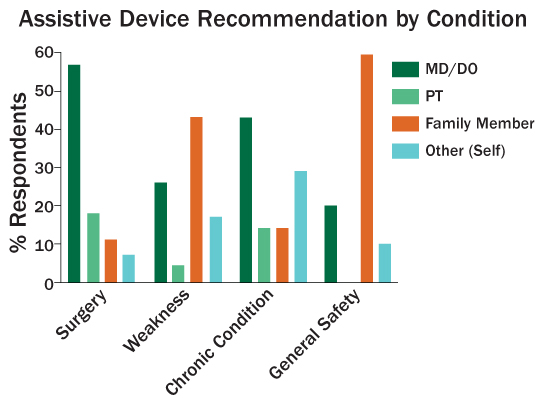
The Right Fit: Closing the Education Gap in Assistive Ambulation Devices Some individuals or groups of individuals within any given community may need varying levels of assistance with ambulation. That assistance can be human or mechanical, but doesn't have to relegate individuals, and by extension communities, to a sedentary, isolated, and often life-threatening lifestyle. According to the National Health and Aging Trends study of 2011–2012, one-quarter (24%) of adults aged 65 and older use a mobility or ambulation assistive device (AAD) such as a cane, crutches, or a walker to ensure a safe, steady gait.1 The need for assistance may be due to impairment of balance, coordination, sensation, or strength or a history of falls. Despite the need for assistance, all people within a given community can be engaged, confident, mobile, and productive if given sufficient knowledge and the proper equipment. Health Literacy and Education An article published in The Gerontologist in 2002 based on Flemish research indicates attitudes run on a continuum. Extremes range from "an [assistive device] gives a person more independence and a great quality of life" to the polar opposite: "I will be perceived as old and sick."3 Assistive Device Access and Education Current literature suggests approximately 30% of patients obtain their assistive devices through a medical professional. The remaining 70%, or a majority of patients, obtain assistive devices on their own or on the advice of family and friends. Additionally, only 20% receive proper education on the purpose and proper use of the device.4 Primary Care Mental health topics tended to dominate office discussion followed closely by biomedical concerns. Tai-Seale and colleagues refer to works by Braddock et al (1999) and Beasley et al (2004) confirming three to four biomedical topics are raised in most office visits. Biomedical concerns would be those that might result in a recommendation for use of an AAD. Recent research also reports that secondary professionals, such as pharmacists who might be involved in direct market access, are poorly educated on AADs and ill equipped to properly and safely recommend a device, fit it to consumers, and educate them about its use.6 If concerns are not properly addressed, this self-selecting population is at greater risk for injury and harm, which could negatively influence both personal and economic well-being. Determining Health Literacy The study population consisted of individuals 65 and older from two senior center programs and one specialized living community in Southern California. A written survey was used to gather information regarding AADs and health education/literacy including the specific device(s) used, who recommended the devices, whether the devices were fitted to the individuals, whether the users were educated about why a particular device was recommended for them, and how they maintain their equipment. A total of 150 surveys were distributed, 80 of which were returned completed, representing a 53% response rate. This study supports the current literature regarding female vs male use of an AAD and the prevalence of walkers vs canes. Specifically, a number of research studies indicate that more women than men use an AAD and that their device of choice is a walker. A previous study placed the number of patients getting their AADs by professional recommendation at 30%. Results from this study indicate 50% of those 65 and older received a recommendation for their AADs from a medical professional. However, as indicated in Figure 1, the remaining 50% of respondents identified as self-prescribers. And as shown in Figure 2, an undeniable trend noted in the results of this study for both genders is that when the need for the devices is related to surgery or chronic conditions, medical personnel were involved. Figure 3 shows that for the remainder of AAD users there may be a perceived need for the AADs by families or the individuals related to the perception of weakness or general safety.
The self-prescriber group was not informed about whether their devices of choice were the best for their particular musculoskeletal, neurological, vestibular, pulmonary, or cardiac situations. Proper fitting of the devices was also questionable. This void of knowledge becomes critical to general health and well-being since 69 of the 80 respondents (86%) reported relying on their devices daily. Other trends emerging from this study include a potential cohort and gender effect. There appears to be a cohort effect among respondents in that the young old (60 to 75) and oldest old (85 and older) reported being "self-prescribers," and a gender gap appears in that females were less likely to be given reasons for a chosen device or to be properly fitted for the device. In addition, office time with one's primary provider regarding diagnosis and AAD was not addressed, nor was interaction with secondary professionals if the AAD was obtained through direct market access. Standards for Recommendations of Devices Samuelsson and Wressle state that the choice of an AAD should be a therapeutic process based on an exchange of information between clinician and patient, client, or resident that includes knowledge and understanding of the following areas: physical, psychological, environmental presuppositions, and needs and priorities of each individual.1 This exchange of information and the level of understanding therein can have positive or negative impacts on one's overall well-being. Due to the high number of patients obtaining their AADs through direct access, secondary level professionals such as pharmacists were surveyed on their education in this area. A 2007 study of 68 pharmacists from Alberta, Canada, revealed that only 5% believed that their training was "definitely sufficient" in AADs. Seventy percent of pharmacists involved in the study indicated they could not describe how to fit an AAD, and more than 50% could not describe how to use the AAD for ambulation. Outcomes from this study resulted in the formulation of an interdisciplinary training module for physical therapy and pharmacy students on assessing, recommending, and fitting AADs acquired via direct market access.7 To enhance the health literacy of practicing pharmacists and protect the well-being of patients seeking direct market access to AADs, the Alberta research team also developed a series of guidelines addressing assessment, measurement, and fitting of AADs, as well as the necessity to refer patients back to an MD, DO, or PT before dispensing the AAD.7 Education "Mobilizing Knowledge: The Evidence Gap for Assistive Devices" cites works from Johnston and colleagues (2009) and the World Health Organization indicating that technology related to rehabilitation is evolving and being marketed to the public by direct access in some cases faster than health professionals and researchers can truly evaluate its safety and proper use with given patient populations.10 Therefore, the article suggests the development of a continuum of information (ie, linear and ongoing resource of current information) that would provide access to a wide scope of knowledge. Two essential areas where education is needed related to AADs are the immediate availability of information about new technologies/devices and the comparison of like items. Such a continuum of information would allow the prescribers and medical suppliers not only to recommend an appropriate piece of equipment but also to provide an evidence-based education to the device users.10 Professional Responsibility The suggestions noted above, combined with basic education materials to increase education regarding AADs in multiple languages (including but not limited to written, audio, and in-person programs), provide a firm foundation. Check-back and teach-back techniques may be helpful in providing valid proof of understanding. Check back is a generalized verbal recount by patients that they understand what instructions were given. Teach back can be verbal or physical. In 2014, 14.5% of the US population—46.3 million people—were age 65 or older.11 Using the National Health and Aging Trends study statistics as a guideline means that approximately 11.5 million older adults use an assistive device. Studies place the range of self-prescribers at 30% to 50%. Based on those averages, from 3.8 million to 5.7 million Americans obtain their devices through direct market access. This results in a huge void in health education. Injury, pain, suffering, and medical expense can be avoided by implementing some of the proposed interventions listed in this article. It's the obligation and responsibility of health care providers to close the education gap. — Celeste R. Dunlap, MSHS, PTA, is a physical therapist assistant with recognition of advanced proficiency in geriatric physical therapy at Casa Colina's Adult Day Healthcare at Casa Colina Hospital and Centers for Healthcare. — Emily R. Rosario, PhD, is a neuroscientist and director of the Research Institute at Casa Colina Hospital and Centers for Healthcare.
References 2. Sudore RL, Yaffe K, Satterfield S, et al. Limited literacy and mortality in the elderly: the health, aging, and body composition study. J Gen Intern Med. 2006;21(8):806-812. 3. Roelands M, Van Oost P, Depoorter A. Buysse A. A social-cognitive model to predict the use of assistive devices for mobility and self-care in elderly people. Gerontologist. 2002;42(1):39-50. 4. Bradley SM, Hernandez CR. Geriatric assistive devices. Am Fam Physician. 2011;84(4):405-411. 5. Tai-Seale M, McGuire TG, Zhang W. Time allocation in primary care office visits. Health Serv Res. 2007;42(5):1871-1894. 6. Sadowski C, Jones A. Ambulatory assistive devices. How to appropriately measure and use canes, crutches and walkers. Pharm Pract. 2014;1(10):24-31. 7. A physiotherapy-pharmacy partnership to move clients. Alberta College of Pharmacy website. https://abpharmacy.ca/articles/physiotherapy-pharmacy-partnership-move-clients. Published April 7, 2009. 8. Waitzkin H. Doctor-patient communication. Clinical implications of social scientific research. JAMA. 1984;252(17):2441-2446. 9. Ong LM, de Haes JC, Hoos AM, Lammes FB. Doctor-patient communication: a review of the literature. Soc Sci Med. 1995;40(7):903-918. 10. Lemaire ED. Mobilizing knowledge: the evidence gap for assistive devices. Technol Innov Manage Rev. 2016;6(9):39-45. 11. Older adults. HealthyPeople.gov website. https://www.healthypeople.gov/2020/topics-objectives/topic/older-adults. Retrieved May 22, 2018. |