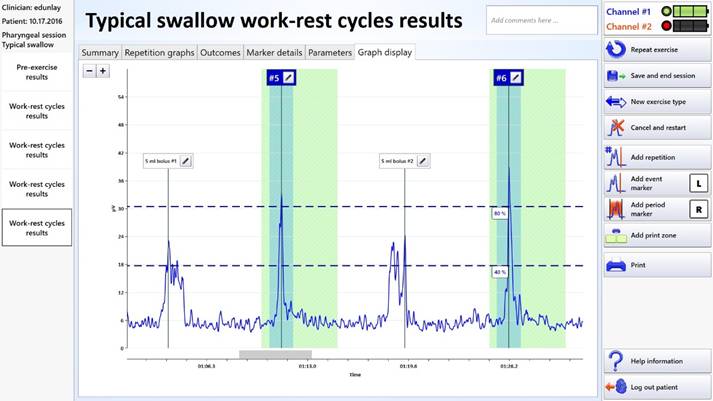
Surface Electromyography Device Assists in Rehabilitation of Swallowing DisordersBy Kristine Galek, PhD, CCC-SLP; Ed M. Bice, MEd, CCC-SLP; and Amy Hobbs, PT, GCS, CEEAA Approximately one in 25 adults will experience some type of swallowing problem. These individuals are at increased risk of dehydration, malnutrition, and pneumonia. In addition, those who suffer from swallowing disorders report a diminished quality of life.1 Swallowing is a complex biomechanical process that is associated with the sequential displacement of the oral pharyngeal structures and bolus transport to the esophagus. Dysphagia is a swallowing disorder that is characterized as a disruption of this biomechanical process. Dysphagia can occur as a result of structural damage, a symptom of a progressive neurological disease, or a traumatic brain injury.2 According to several epidemiologic reports, 38% of older adults living at home, 68% of institutionalized dementia patients, 60% of patients recovering from head and neck cancer surgery, 80% with late-stage Parkinson's disease, and 78% of an estimated 600,000 patients who are impaired by a stroke each year, suffer from some degree of swallowing impairment.3 The consequences of dysphagia can be profound, resulting in compromised nutritional status, dehydration, diminished quality of life, and social isolation. In addition, aspiration and subsequent pneumonia may be a pivotal factor that precipitates poor outcomes in ill or frail individuals.4 Speech language pathologists typically provide a skilled assessment and intervention to patients who present with dysphagia. Appropriate direct and indirect interventions can include behavioral, dietary, medical, and surgical recommendations. Speech pathologists typically target swallowing disorders with behavioral treatment designed to rehabilitate disordered swallow physiology. The behavioral swallow interventions can consist of compensatory strategies, postural changes, resistive tongue and lip exercise, and appropriate swallow maneuvers that involve principles of motor planning, neuroplasticity, and strengthening.5 Dysphagia Treatment In addition to adequate strength and range of motion, effective swallowing requires neuromuscular coordination, precise timing, and proper planning and precision of motor movements. An important element for motor learning is feedback concerning task performance. During execution of motor tasks, visual feedback and proprioceptive awareness are coupled with kinesthetic feedback and transmitted to the central nervous system. If the projected plan and actual performance differ, a correction process influences the subsequent trial. Improved performance is influenced by feedback.7 Because swallowing produces no clear visually observable movement patterns, information provided by augmented feedback provides a necessary component for improving swallowing performance.8 Adjunctive surface electromyography (sEMG) is a noninvasive visual and auditory biofeedback tool that measures electrical muscle activity through the use of self-adhesive hydrogel electrodes. The electrodes are applied to the skin over the appropriate muscles. The muscle activity is captured by the electrodes and transmitted to a computer. The computer processes the transmitted information into visualizations of muscle activity that can be used by the clinician and patient to assist in modifying the swallow behavior. Crary et al reported that inexperienced clinicians demonstrate acceptable accuracy and reliability in the identification of swallows from sEMG traces.9 Reliability was acceptable because normal swallowing presents a robust and distinct sEMG signal that is easily distinguished from background activity. In addition, the study indicated that both sensitivity and specificity improved with use (0.87 and 0.97 for experienced raters vs 0.79 and 0.9 for naïve raters). Studies suggest that with appropriate intensive short-term treatment (9 to 15 days) augmented by sEMG, patients are often able to return to functional oral intake. Synchrony The virtual reality augmented sEMG biofeedback enables speech language pathologists and patients to effectively use virtual reality activities to visualize therapeutic swallowing activity. The virtual reality activities include work-rest cycles, the diver, the kangaroo, and the bow-and-arrow visualizations, shown below. These visualizations can be used for training novel maneuvers, visualizing swallow repetitions, teaching and cueing motor planning, practicing neuroplasticity principles and implementing skill-based learning techniques. As a patient improves, a clinician can manipulate the visualizations and progressively make the tasks more therapeutically challenging. Research demonstrates that virtual reality exercise can enhance therapy outcomes, as patients are typically distracted from the exercise and work at greater intensities for longer periods of time.10 The "Work-Rest Cycle" is designed to improve swallow coordination and timing. Figure 1: Synchrony Work-Rest Cycle
The Diver activity is designed to target tongue base retraction, endurance, and specificity of lingual movement. Figure 2: Synchrony Diver Activity
Additionally, the Kangaroo activity is designed to target strength, duration, and progressive resistance. Figure 3: Synchrony Kangaroo Activity
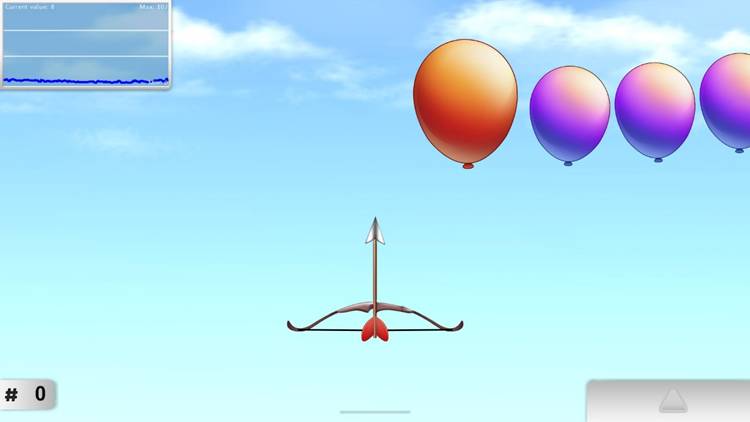
Figure 4: Synchrony Bow and Arrow Activity
Synchrony is currently being used in more than 500 sites including skilled nursing facilities, inpatient rehabilitation facilities, and outpatient centers as well as university labs and clinics. Continual collection of feedback from front-end users and collaboration with well-respected dysphagia researchers enhances the utility and performance of Synchrony. — Kristine Galek, PhD, CCC-SLP, is an assistant professor of speech-language pathology at the University of Nevada, Reno, codirector of Northern Nevada Voice and Swallow Clinic and director of the RAVSS Research Laboratory. She is a practicing clinician with 20 years of dysphagia experience. Her clinical and research interests focus on swallowing, voice, and resonance disorders. — Ed M. Bice, MEd, CCC-SLP, is a speech-language pathologist with experience in acute care, outpatient, home health, and skilled nursing. He serves as associate editor for the American Speech-Language-Hearing Association's gerontology special interest group and clinical program consultant for Accelerated Care Plus' Synchrony dysphagia program. 2. Lazarus C, Logemann JA. Swallowing disorders in closed head trauma patients. Arch Phys Med Rehabil. 1987;68(2):79-87. 3. Layne KA, Losinski DS, Zenner PM, Ament JA. Using the Fleming Index of Dysphagia to establish prevalence. Dysphagia. 1989;4(1):39-42. 4. Altman K, Yu G, Schaefer S. Consequence of dysphagia in the hospitalized patient i: mpact on prognosis and hospital resources. Arch Otolaryngol Head Neck Surg. 2010;136(8):784-789. 5. Burkhead LM, Sapienza CM, Rosenbeck JC. Strength-training exercise in dysphagia rehabilitation: principles, procedures and direction for future research. Dysphagia. 2007;22(3):251-265. 6. Logemann J. Evaluation and Treatment of Swallowing Disorders. San Diego: College-Hill Press; 1983. 7. Salmoni AW, Schmidt RA, Walter CB. Knowledge of results and motor learning: a review and critical reappraisal. Psychol Bull. 1984;95(3):355-386. 8. Athukorala R, Jones R, Sella O, Huckabee M. Skill training for swallowing rehabilitation in patients with Parkinson's disease. Arch Phys Med Rehabil. 2014;95(7):1374-1382. 9. Crary M, Carnaby Mann G, Groher M. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005;86(8):1516-1520. 10. Corbetta D, Imeri F, Gatti R. Rehabilitation that incorporates virtual reality is more effective than standard rehabilitation for improving walking speed, balance and mobility after stroke: a systematic review. J Physiother. 2015;61(3):117-124. |