July/August 2016
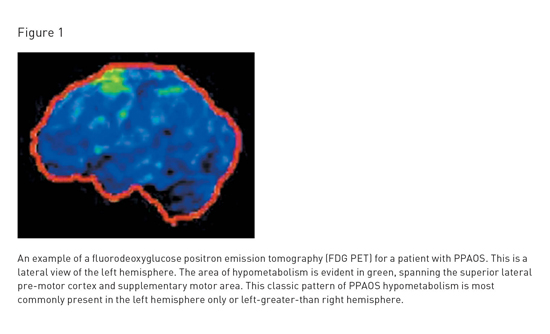
Primary Progressive Apraxia of Speech Using speech to communicate requires a complex series of actions that begins with selecting appropriate words and organizing them into grammatical sentences. This internally formulated message is then executed as speech through "speech programming," a crucial subconscious process that creates and conveys instructions for movements of about 100 muscles between the lungs and lips. For adult speakers, this results in the production of at least 14 distinct speech sounds per second. When the brain and body systems are intact, this extraordinarily complex speech act occurs effortlessly. Unfortunately, spoken communication can break down in several ways. In aphasia, the ability to select and organize words may be compromised. In what is called dysarthria, language function is preserved, but the speech muscles themselves may be compromised by weakness, spasticity, incoordination, or involuntary movements. When the speech programming stage is affected, the problem is called apraxia of speech. These problems may or may not be isolated and, unfortunately, any one of them can have devastating consequences on the ability to communicate. Speech problems like those described above are often associated with stroke or other traumatic brain injuries. However, they may also be a first and early sign of neurodegenerative disease, a possibility that is often underrecognized by the general public and nonspecialists in medicine. Recently, accumulating research has helped in understanding a neurodegenerative condition that manifests first, or primarily, as apraxia of speech. On average, it takes between 21/2 and three years between initial symptom onset and a diagnosis of primary progressive apraxia of speech (PPAOS). The delay in proper diagnosis can be attributed to a lack of awareness of this condition among both the general public, who, initially at least, may attribute its symptoms to stress or fatigue, and among health care providers, who often misdiagnose this difficulty as aphasia or dysarthria. There is evidence to suggest PPAOS is not as rare as it was once thought, potentially because of misdiagnoses as a functional/psychogenic problem, a variant of aphasia, or another neurodegenerative disease, such as Alzheimer's disease or amyotrophic lateral sclerosis (ALS). What Is PPAOS (and What Is It Not)? Recent research has established that a subset of people who in the past have been classified as having PPA (nonfluent subtype) actually do not have aphasia at all. They can read, write, comprehend speech, and find words and organize grammatical sentences, but instead are unable to program speech movements. This subset of people instead has PPAOS. Importantly, this diagnosis is appropriate only when apraxia of speech is the first, the only, or the most salient feature and there are no additional problems that would meet criteria for a more specific neurologic diagnosis.3 Among even expert neurologists and speech-language pathologists, AOS can be difficult to distinguish from other speech and language disorders. This includes its distinction from aphasia. AOS is often overlooked or ignored in patients who receive an aphasia diagnosis, even though one diagnosis does not preclude the other, and they often co-occur. The diagnostic challenge is especially true when aphasia presents as nonfluent or hesitant speech as a result of word-finding deficits or difficulty with grammar. This is in contrast to the delays for speech production seen secondary to restarts and revisions associated with AOS. Furthermore, distorted sound substitutions, secondary to abnormal motor planning, are also often misconstrued as errors associated with aphasia. AOS can be confused with dysarthria, which arises from a disruption of the neuromuscular control of speech rather than the inability to generate motor programs for speech movement. For instance, speech may present as segmented and slowed in association with ataxic or spastic dysarthria due to cerebellar or upper motor neuron damage, respectively. However, there are many features suggestive of apraxia of speech that are not present when dysarthria is the accurate and sole diagnosis.4 Some examples of other diagnostic labels that are roughly synonymous with PPAOS include slowly progressive anarthria (or dysarthria), progressive aphemia, phonetic disintegration, buccofacial apraxia, and anterior opercular syndrome. Who Is Affected by PPAOS? How Is PPAOS Identified? Research by the authors suggests that there may be subtypes of PPAOS.5 In what the authors call type 1, speech is dominated by difficulty with articulation (ie, productions of speech sounds), with distorted sound substitutions, and stop and start attempts to correct errors, including audible or visible groping. That pattern of difficulty tends to be more evident when aphasia is also present. In what the authors call type 2, there are predominant prosodic abnormalities, with slowed speaking rate and segmentation between syllable and words; however, there is relatively less difficulty with articulation, as in type 1. The type 2 pattern tends to be more evident in PPAOS. In the Type 3 pattern, there is no clear predominance of the articulatory vs prosodic abnormalities; they are both nearly equally evident. Assessment and characterization of speech patterns is critical in guiding diagnosis, but neuroimaging is also helpful for confirming the diagnosis. An example of key neuroimaging findings associated with PPAOS and PPA is presented in Figure 1.6
Pathophysiology of PPAOS What Is the Prognosis and Treatment for PPAOS? In some patients, severe parkinsonism, vertical eye gaze problems, urinary incontinence, balance difficulty with falls, swallowing problems, or limb apraxia develop; these findings are similar to a neurodegenerative condition known as progressive supranuclear palsy.9 In another subset of patients, asymmetric rigidity of the extremities, alien limb, limb apraxia, and other parkinsonian features may emerge, similar to another neurodegenerative condition known as corticobasal syndrome.10 Although there is typically no evidence of memory loss, impulsivity, or other neuropsychological or neurobehavioral deficits early in the disease course, they may become evident over time.11 Available Treatments for PPAOS — Rene Utianski, PhD, is a clinical postdoctoral fellow in speech-language pathology at Mayo Clinic in Rochester, Minnesota, and an assistant professor of neurology at the Mayo Clinic College of Medicine. — Joseph Duffy, PhD, is an emeritus consultant of speech pathology in the department of neurology at Mayo Clinic in Rochester, Minnesota, and professor of speech pathology at the Mayo Clinic College of Medicine. — Keith Josephs, MD, is a consultant of neurology at Mayo Clinic in Rochester, Minnesota, and professor of neurology at the Mayo Clinic College of Medicine. He is the principal investigator of many National Institutes of Health-funded grants including a grant to study primary progressive aphasia and primary progressive apraxia of speech. References 2. Gorno-Tempini ML, Hillis AE, Weintraub S, et al. Classification of primary progressive aphasia and its variants. Neurology. 2011;76(11):1006-1014. 3. Josephs KA, Duffy JR, Strand EA, et al. Characterizing a neurodegenerative syndrome: primary progressive apraxia of speech. Brain. 2012;135(Pt 5):1522-1536. 4. Duffy JR. Apraxia of speech in degenerative neurologic disease. Aphasiology. 2006;20(6):511-527. 5. Josephs KA, Duffy JR, Strand EA, et al. Syndromes dominated by apraxia of speech show distinct characteristics from agrammatic PPA. Neurology. 2013;81(4):337-345. 6. Josephs KA, Duffy JR, Fossett TR, et al. Fluorodeoxyglucose F18 positron emission tomography in progressive apraxia of speech and primary progressive aphasia variants. Arch Neurol. 2010;67(5):596-605. 7. Josephs KA, Duffy JR, Strand EA, et al. Clinicopathological and imaging correlates of progressive aphasia and apraxia of speech. Brain. 2006;129( Pt 6):1385-1398. 8. Deramecourt V, Lebert F, Debachy B, et al. Prediction of pathology in primary progressive language and speech disorders. Neurology. 2010;74(1):42-49. 9. Josephs KA, Duffy JR. Apraxia of speech and nonfluent aphasia: a new clinical marker for corticobasal degeneration and progressive supranuclear palsy. Curr Opin Neurol. 2008;21(6):688-692. 10. Josephs KA, Boeve BF, Duffy JR, et al. Atypical progressive supranuclear palsy underlying progressive apraxia of speech and nonfluent aphasia. Neurocase. 2005;11(4):283-296. 11. Duffy JR, Peach RK, Strand EA. Progressive apraxia of speech as a sign of motor neuron disease. Am J Speech Lang Pathol. 2007;16(3):198-208. |