July/August 2017
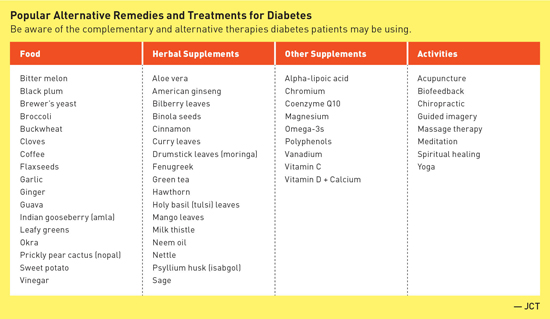
Top 5 Alternative Diabetes Therapies: Are Patients Undermining Their Treatment? Patients with diabetes are turning to unregulated and understudied supplements, foods, and other alternative treatments. Although some may prove useful, others carry risk of real harm. Many individuals with diabetes are turning to home remedies and alternative treatments in an attempt to mitigate their chronic illness or prevent complications.1 Older adults are particularly at risk from unscrupulous schemes and fraudulent health claims.2 The long history of food and herbal diabetes treatments in many cultures, combined with a general rise in the use of complementary and alternative medicine (CAM) over the last few decades makes it likely that many patients are trying one or more of these remedies.3 The popularity of herbal remedies, supplements, and food "cures" certainly doesn't guarantee their safety.1 Adverse effects and interactions are possible, and patients on insulin or secretagogues (such as sulfonylureas and glinides) are at increased risk for hypoglycemia when using CAM therapies.3 A 2017 study found higher CAM use resulted in lower quality of life in people with type 2 diabetes, possibly as a result of the negative effects of using multiple therapies and their interactions with conventional care. Additionally, diabetes patients using CAM showed decreased adherence to prescribed medications.3 Complementary and alternative treatments can take the form of foods, herbal remedies, supplements, activities, or even illegally marketed diabetes drugs. Below is a detailed description of a popular choice in each of these categories. 1. Food: Apple Cider Vinegar Research vs Hype It is theorized that vinegar might slow the digestion of starches, delay the emptying of food from the stomach, or alter glucose production in the liver, and a small 2015 study found that, compared with a placebo, vinegar increased glucose uptake by muscles.6,7 Unfortunately the blood sugar control effect of vinegar appears to be strongest in people who do not have diabetes or prediabetes.8 Cautions 2. Herbal Remedy: Cinnamon Research vs Hype In late 2016, another group of researchers attempted a meta-analysis but concluded that the existing studies were too heterogeneous to be analyzed together. In reviewing the 11 randomized controlled trials involving nearly 700 adults with type 2 diabetes, the authors concluded that cinnamon supplements added to standard hypoglycemic medications and other lifestyle therapies had modest effects on fasting plasma glucose and hemoglobin A1c, but they stopped short of recommending its use until larger and more rigorous studies are available. Cinnamon doses in the studies reviewed ranged from 120 mg to 6,000 mg per day.12 "Cinnamon may be of some slight benefit in lowering blood sugar," says Marina Chaparro, MPH, RDN, CDE, a spokesperson for the Academy of Nutrition and Dietetics, "but there is not enough research to recommend its use." In fact, the National Center for Complementary and Integrative Health concluded in 2016 that human studies don't support using cinnamon for any health condition, and the American Diabetes Association does not recommend cinnamon's use in diabetes treatment.13,14 Cautions 3. Supplement: Chromium Research vs Hype Cautions 4. Activity: Yoga Research vs Hype Cautions 5. Illegally Marketed Drugs Research vs Hype Cautions
Talking to Patients Once patients have opened up about their activities, Sturner recommends open-ended questioning. "Listen, be understanding, and ask open-ended questions," Sturner says, such as, "Can you tell me why you chose to take that? Has it made a difference?" Chaparro recommends providing patients the information they need to understand the impact of what they are doing. "Get back to basics," Chaparro says. "Let them understand how their body works, and what this treatment might do." Emphasizing the need for evidence-based practice may help. "We explain that we put patient safety first," Sturner says, "and go over what the evidence says about risks and benefits." Many CAM treatments may be harmless, and preliminary research indicates some may be helpful, but the potential for undesirable interactions with conventional medicines, possible adverse effects, and the risk that patients will abandon effective treatments for the promise of a 'natural' cure make it imperative that health care providers be aware of common alternative treatments and enable open communication with their diabetes patients.1 — Judith C. Thalheimer, RD, LDN, is a registered dietitian and principal of JTRD Nutrition Education Services, LLC, outside Philadelphia.
TIPS FOR SAFE USE OF COMPLEMENTARY THERAPIES • Avoid drug interactions. Encourage patients to inform all of their health care professionals about any and all complementary treatments they are trying and to continue to take conventional medication as prescribed. • Buy supplements and drugs from a trusted source. Supplements are unregulated. Urge patients to look for a US Pharmacopeial Convention seal on packaging to ensure that supplements come from a reputable source. More information is available at www.quality-supplements.org. To ensure an online pharmacy is legitimate, the FDA recommends the following: • Ensure the site requires a valid prescription. • Take a systematic approach. If a patient wants to try a supplement or treatment (and it can be determined that this treatment is not dangerous or detrimental to health), suggest trying it for a limited period of time. Work with patients to determine whether A1c, blood sugar control, or quality of life has improved after the trial period. • Monitor kidney and liver function. Patients may not realize that "natural" remedies can have adverse effects. Recommend laboratory tests for kidney and liver function to ensure the supplement is not harming the patient's health. — Sources: http://www.diabetesforecast.org/2012/feb/the-pros-and-cons-of-dietary-supplements.html; https://www.fda.gov/forconsumers/consumerupdates/ucm361487.htm
References 2. Scams and safety: fraud against seniors. FBI website. https://www.fbi.gov/scams-and-safety/common-fraud-schemes/seniors 3. Kesavadev J. Efficacy and safety concerns regarding complementary and alternative medicine use among diabetes patients. J Pak Med Assoc. 2017;67(2):316-319. 4. Johnston CS, Kim CM, Buller AJ. Vinegar improves insulin sensitivity to a high-carbohydrate meal in subjects with insulin resistance or type 2 diabetes. Diabetes Care. 2004;27(1):281-282. 5. Shishehbor F, Mansoori A, Shirani F. Vinegar consumption can attenuate postprandial glucose and insulin responses; a systematic review and meta-analysis of clinical trials. Diabetes Res Clin Pract. 2017;127:1-9. 6. Weisenberger J. Vinegar: a diabetes do or don't? Diabetes Forecast. November 2014. http://www.diabetesforecast.org/2014/11-nov/vinegar-a-diabetes-do-or.html?loc=ymal 7. Mitrou P, Petsiou E, Papakonstantinou E, et al. Vinegar consumption increases insulin-stimulated glucose uptake by the forearm muscle in humans with type 2 diabetes. J Diabetes Res. 2015;2015:175204. 8. Lim J, Henry CJ, Haldar S. Vinegar as a functional ingredient to improve postprandial glycemic control-human intervention findings and molecular mechanisms. Mol Nutr Food Res. 2016;60(8):1837-1849. 9. Find a vitamin or supplement: apple cider vinegar. WebMD website. http://www.webmd.com/vitamins-supplements/ingredientmono-816-APPLE+CIDER+VINEGAR.aspx 10. Cotey S, Harris A. Can taking cinnamon supplements lower your blood sugar? Cleveland Clinic website. https://health.clevelandclinic.org/2016/10/can-taking-cinnamon-lower-your-blood-sugar/. Published October 4, 2016. 11. Allen RW, Schwartzman E, Baker WL, Coleman CI, Phung OJ. Cinnamon use in type 2 diabetes: an updated systematic review and meta-analysis. Ann Fam Med. 2013;11(5):452-459. 12. Costello RB, Dwyer JT, Saldanha L, Bailey RL, Merkel J, Wambogo E. Do cinnamon supplements have a role in glycemic control in type 2 diabetes? A narrative review. J Acad Nutr Diet. 2016;116(11):1794-1802. 13. Cinnamon. National Center for Complementary and Integrative Health website. https://nccih.nih.gov/health/cinnamon. Updated November 29, 2016. 14. Cinnamon. WebMD website. http://www.webmd.com/diet/supplement-guide-cinnamon. Updated March 8, 2017. 15. Graedon T. Which cinnamon is better for blood sugar? The People's Pharmacy website. https://www.peoplespharmacy.com/2016/08/01/which-cinnamon-is-better-for-blood-sugar/. Published August 1, 2016. 16. Herbs, supplements and alternative medicines. American Diabetes Association website. http://www.diabetes.org/living-with-diabetes/treatment-and-care/medication/other-treatments/herbs-supplements-and-alternative-medicines/#sthash.P7FlXEUn.dpuf. Updated February 20, 2014. 17. Diabetes and dietary supplements: in depth. National Center for Complementary and Integrative Health website. https://nccih.nih.gov/health/diabetes/supplements. Updated June 23, 2016. 18. Anderson RA. Chromium and parenteral nutrition. Nutrition. 1995;11(1 Suppl):83-86. 19. Suksomboon N, Poolsup N, Yuwanakorn A. Systematic review and meta-analysis of the efficacy and safety of chromium supplementation in diabetes. J Clin Pharm Ther. 2014;39(3):292-306. 20. Costello RB, Dwyer JT, Bailey RL. Chromium supplements for glycemic control in type 2 diabetes: limited evidence of effectiveness. Nutr Rev. 2016;74(7):455-468. 21. Chromium dietary supplement fact sheet. National Institutes of Health website. https://ods.od.nih.gov/factsheets/Chromium-HealthProfessional/. Updated November 4, 2013. 22. Yoga as a complementary health approach. National Center for Complementary and Integrative Health website. https://nccih.nih.gov/news/multimedia/infographics/yoga. Updated March 15, 2016. 23. Cui J, Yan JH, Yan LM, Pan L, Le JJ, Guo YZ. Effects of yoga in adults with type 2 diabetes mellitus: a meta-analysis. J Diabetes Investig. 2017;8(2):201-209. 24. Vizcaino M, Stover E. The effect of yoga practice on glycemic control and other health parameters in type 2 diabetes mellitus patients: a systematic review and meta-analysis. Complement Ther Med. 2016;28:57-66. 25. Yoga: in depth. National Center for Complementary and Integrative Health website. https://nccih.nih.gov/health/yoga/introduction.htm. Updated September 26, 2016. 26. Paturel A. Yoga poses for your 50s, 60s and 70s — and beyond. AARP Magazine. November 2016. http://www.aarp.org/health/healthy-living/info-11-2013/health-benefits-of-yoga.html 27. Beware of illegally marketed diabetes treatments. US Food & Drug Administration website. https://www.fda.gov/ForConsumers/ConsumerUpdates/ucm361487.htm. Updated November 10, 2016. |