July/August 2017
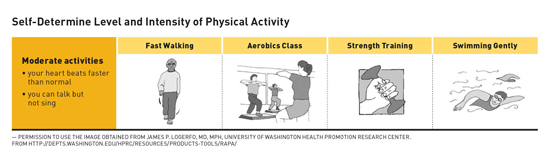
Study Reinforces Walking's Heart Health Benefit A community walking program utilizing pedometers with tracking capabilities successfully improved cardiovascular risk factors in a group of older rural women studied for the program. The World Health Organization reports that cardiovascular disease (CVD) is the leading cause of death worldwide.1 If behavioral risk factors such as physical activity, weight, and smoking are modified, most CVDs can be prevented.1,2 Recommendations on physical activity include a discussion of health benefits with moderately intense physical activity of at least 150 minutes per week.1,3 Evidence also suggests that a routine of brisk walking qualifies as moderate-intensity physical activity.3 A relationship between increased physical activity and decreased risk of CVD has been shown.1,3 A study conducted in a rural community sought to determine whether cardiovascular risk factors could be reduced in females who participated in a 10-week pedometer-based walking program.4 The effects of this walking program were examined by evaluating pre- and postblood pressure (BP), total cholesterol (TC), high-density lipoprotein (HDL), weight, body mass index (BMI), 10-year cardiovascular risk, and results of a six-minute walk test. Researchers, including the authors, also evaluated the effects of the use of a pedometer with tracking capability and the use of a raffle incentive. Data were analyzed via descriptive statistics and eight paired t-tests of pre- and postdata. Females in the rural community were targeted for this study because heart disease is the leading cause of mortality among women.2,4 Seventy women began the program, with 62 completing it, providing a retention rate of 88%. Most analysis included 60 subjects due to incomplete data on two women. The average and median ages for women in the study were 55 and 59 years, respectively, with a range of 50 years spanning ages from 29 to 79. The sample was 100% white. Participants were recruited for the research study from individuals who had signed up for a community walking program. Height, weight, age, BMI, and BP were initially obtained to determine eligibility. Data collection took place over the summer at the local college. Women were eligible to participate if they were older than 18 with one or more of the following criteria: BMI >24 kg/m2, systolic blood pressure (SBP) <160 mm Hg, diastolic blood pressure (DBP) <100 mm Hg, current tobacco use or use within the past year, and/or sedentary lifestyle the previous two years by self-report. Exclusion criteria included having had surgery to promote weight loss, BMI >40 kg/m2; SBP >160 mm Hg; DBP >100 mm Hg; and history of heart failure, stroke, or inability to exercise. Women who met inclusion criteria were offered the opportunity to participate in the study. Participants were each given a pedometer to wear during waking hours over the course of the 10-week period. The pedometers were capable of recording and storing activity data that could later be downloaded to a computer. Pedometers were set up by a research assistant to ensure proper functioning. Participants were asked to walk briskly for at least 150 minutes per week. A web-based Framingham Heart Study risk assessment tool including data on age, total cholesterol, HDL cholesterol, SBP, smoking status, and BP medication status was used to determine a participant's CVD risk for having a heart attack within 10 years.5 The principal investigator reviewed the pedometer activity data with the participants at week five. Participants were further offered a challenge to increase their total daily average of aerobic steps by at least 10% for the remainder of the study in order to be entered into a drawing for a gift certificate. This challenge was offered to increase aerobic activity as well as to improve retention to study completion. Final data were collected at 10 weeks. Cohort of Women Aged 55 and Older
The pretest physiological measurements for this cohort included a mean BMI of 29.71 kg/m2 with a range from 21.7 to 43.8 kg/m2. Per the National Heart, Lung, and Blood Institute, a BMI >30 kg/m2 is considered obese.6 The mean weight was 171 lbs, with the range from 111 lbs to 263 lbs. The mean SBP was 134 mm Hg; mean DBP was 79 mm Hg. Twenty-three participants (61%) reported taking BP medication compared with 27 (44%) of the entire sample, which included the younger participants. The mean TC was 208, and the mean HDL was 57. Twelve participants (32%) of the older cohort reported taking lipid-lowering medication, compared with 15 (24%) of the entire sample. The mean 10-year CVD risk score was 4% for the older group and 3% for the full study.4 Posttest results for the older cohort showed a statistically significant improvement (p<0.05) in weight, BMI, total cholesterol, SBP, and the six-minute walk test. Although not statistically significant, there was also an improvement in DBP, HDL, and 10-year CVD risk score. After the incentive raffle challenge was implemented, the women more than doubled their aerobic minutes (p<0.05) from midway through to the end of the study. These findings mirrored those of the larger sample.4 This study provided a sound short-term intervention for implementation in similar rural populations. Study Limitations Implications and Recommendations for Practice Conclusion — Elisabeth Marigliano, BS, RN, is an adjunct clinical faculty member in the School of Nursing at State University of New York at Delhi and a PhD student at Binghamton University, State University of New York. — Pamela Stewart Fahs, PhD, RN, is a professor and associate dean of nursing at Binghamton University, State University of New York, Decker School of Nursing. She holds the Dr. G. Clifford and Florence B. Decker Chair in Rural Nursing.
References 2. Fahs PS, Pribulick M, Williams IC, James GD, Rovynak V, Seibold-Simpson SM. Promoting heart health in rural women. J Rural Health. 2013;29(3):248-257. 3. US Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. https://health.gov/paguidelines/pdf/paguide.pdf 4. Marigliano E, Fahs PS, Ludden C. Walking for heart health: a study of adult women in rural New York. Creat Nurs. 2016;22(4):268-275. 5. Estimate of 10-year risk for coronary heart disease Framingham point scores. National Heart, Lung, and Blood Institute website. https://www.nhlbi.nih.gov/health-pro/guidelines/current/cholesterol-guidelines/quick-desk-reference-html/10-year-risk-framingham-table#women. Accessed April 1, 2017. 6. Body mass index (BMI) chart. National Heart, Lung, and Blood Institute website. https://www.nhlbi.nih.gov/files/docs/resources/heart/filipino-health-manual/session-6/bmi.pdf. Accessed April 1, 2017. 7. What is 'Script Trails? Prescription Trails Delaware County website. http://getoutandwalk.org/what-is-script-trails/. Accessed April 1, 2017. 8. Perri MG, Limacher MC, Durning PE, et al. Extended-care programs for weight management in rural communities: the treatment of obesity in underserved rural settings (TOURS) randomized trial. Arch Intern Med. 2008;168(21):2347-2354. 9. Shaw R, Fenwick E, Baker G, McAdam C, Fitzsimons C, Mutrie N. 'Pedometers cost buttons': the feasibility of implementing a pedometer based walking programme within the community. BMC Public Health. 2011;11:200. 10. Warren BS, Maley M, Sugarwala LJ, Wells MT, Devine CM. Small Steps Are Easier Together: a goal-based ecological intervention to increase walking by women in rural worksites. Prev Med. 2010;50(5-6):230-234. |