July/August 2018
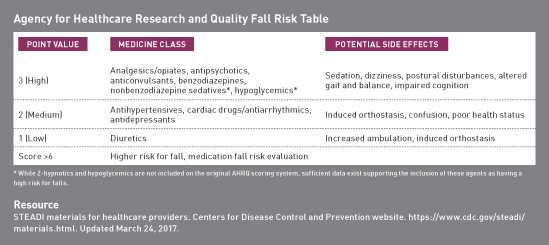
Medication Monitor: Medications That Increase Fall Risk Every second in the United States, an older adult falls, making falls the No. 1 cause of injuries and deaths from injury among older Americans. In fact, more than 1 in 4 older people fall each year. Falls often lead to hospitalizations, hip fractures and other significant injuries, and loss of independence leading to nursing home admission.1 The etiology of falls in older adults is usually multifactorial and may include increasing age, female sex, chronic conditions, and medication use, among others. Most falls are a result of a combination of risk factors. The more risk factors individuals have, the greater their chances of falling.1 Health care providers can help reduce older adults' fall risk by recognizing the use of medications that put patients at high risk of falls and taking steps to minimize their use whenever possible. STEADI Initiative The initiative encourages providers to take the following three initial steps to begin addressing their patients' fall risks related to medications2: • screen to identify patients at risk for a fall; Medication Reviews Determining Medication Fall Risk
Understanding Medication Fall Mechanisms Psychotropic Drugs Anxiolytics/Sedative-Hypnotics BZD use continues to be widespread despite numerous guidelines recommending against it in older adults due to the risk of cognitive impairment, unsteady gait, psychomotor impairment, accidents, delirium, and dependence, which develops quickly.6 Most studies show a significant association between BZD and Z-hypnotic use and falls or fractures.7 Pharmacological alternatives to BZDs for anxiety may include SSRI or SNRI antidepressants.6 While these antidepressants may also increase fall risk, their side effect profiles are considered to be significantly safer than BZDs. Another option for anxiety is buspirone (BuSpar), which has less effect on fall risk and no concerns with dependence. Sleep hygiene and behavioral interventions are recommended as first-line treatments for insomnia, while managing the underlying cause of insomnia (eg, pain, depression).6 Melatonin, which poses significantly less fall risk than do BZDs and Z-hypnotics, may be appropriate for many older adults if needed. Antipsychotics It's important to carefully evaluate the need for antipsychotics and consider tapering or discontinuance as possible by 10% to 25% of the dose per week. The goal is to minimize total psychoactive load, use for shortest period of time, and taper to avoid adverse withdrawal effects. Antidepressants Sedating Antidepressants Common TCAs include amoxapine, desipramine (Norpramin), doxepin, imipramine (Tofranil), and nortriptyline (Pamelor). All of the TCAs should be avoided in older adults due to their side effect profiles. Common antidepressants, including mirtazapine (Remeron) and trazadone, which have chemical structures similar to TCAs but different overall side effect profiles, can also increase fall risk. Selective Serotonin Reuptake Inhibitors (SSRIs) Serotonin Norepinephrine Reuptake Inhibitors (SNRIs) When prescribing any antidepressant, always use the lowest dose needed. Also, try to avoid the concomitant use of other medications with known fall risk, but if such medications are required, prescribe them at the lowest possible dose. Anticholinergic Medications and Side Effects Sedating antihistamines are anticholinergic medications and should be avoided in older adults. These include bropheniramine, chlorpheniramine, cyproheptadine, diphenhydramine, doxylamine, and hydroxyzine. Alternative treatments for allergies include nasal saline, nasal steroids, and second-generation antihistamines (eg, cetirizine, fexofenadine, loratadine). Antihistamines are sometimes used for sleep, which is not advised due to the anticholinergic side effects and fall risk, especially in older adults. For sleep, consider nonpharmacologic interventions and melatonin. Nonpharmacologic interventions are the recommended first-line treatment, but if interventions are not successful, then melatonin may be useful as a pharmacological alternative. Cardiovascular Drugs Cardiovascular drugs generally contribute to falls as a result of hypotension (low blood pressure), orthostatic hypotension (sudden drop in blood pressure upon standing), syncope (fainting), or presyncope (state of lightheadedness, muscular weakness, blurred vision, and feeling faint from carotid sinus hypersensitivity or vasovagal syncope). Stopping cardiovascular medications reduces syncope and falls by 50%. Antihypertensives Alpha-blockers such as doxazosin, prazosin, and terazosin cause blood vessels to dilate, thereby lowering blood pressure. They commonly cause orthostatic hypotension. Giving alpha-blockers at bedtime is a strategy to help reduce fall risk. These agents are also used to treat prostate enlargement in men. An alternative treatment of benign prostatic hypertrophy would be the use of the selective alpha-blocker tamsulosin (Flomax), which has less potential for blood pressure lowering and orthostatic hypotension.6 The centrally acting alpha-2 receptor agonist clonidine (Catapress) may cause severe orthostatic hypotension in addition to bradycardia and potential central nervous system adverse events. In older adults, clonidine use should be avoided.6 Diuretics Thiazide diuretics include chlorthalidone, metolazone, and hydrochlorothiazide. Loop diuretics, which are more potent than thiazide diuretics, include furosemide and bumetanide. Pain Medications A recent study found recent opioid use to be associated with an increased risk of falls and an increased risk of death in older adults. The study included data on 67,929 patients ages 65 and older who were admitted for injury to one of 57 trauma centers. The mean age of patients was 81 years, with more than 69% being women. Falls were the most common cause of injury (92% of patients), and more than one-half (59%) had surgery for their injuries, with lengthy hospital stays (median stay of 12 days). Researchers looked at opioid prescriptions in the preceding two weeks before injury and found that the patients who had filled an opioid prescription during this period were 2.4 times more likely to have had a fall that caused injury. Patients whose falls were linked to opioid use were also more likely to die during their hospital stay.10 Anticonvulsants — Mark D. Coggins, PharmD, BCGP, FASCP, is vice president of pharmacy services and medication management for Diversicare, which operates skilled nursing centers in 10 states. He was nationally recognized by the Commission for Certification in Geriatric Pharmacy with the 2010 Excellence in Geriatric Pharmacy Practice Award. References 2. STEADI materials for healthcare providers. Centers for Disease Control and Prevention website. https://www.cdc.gov/steadi/materials.html. Updated March 24, 2017. 3. Coggins MD. Deprescribing improves quality of life. Today's Geriatr Med. 2017;10(4):8-12. 4. Preventing falls in the hospital. Agency for Healthcare Research and Quality website. https://www.ahrq.gov/professionals/systems/hospital/fallpxtoolkit/fallpxtk-tool3i.html. Updated January 2013. 5. Darowski A, Dwight J, Reynolds J, Radcliffe J; British Geriatrics Society. Medicines and falls in hospitals. www.bgs.org.uk/campaigns/fallsafe/Falls_drug_guide.pdf. Published March 2011. 6. American Geriatrics Society. Updated AGS Beers Criteria. https://geriatricscareonline.org/ProductAbstract/beers-criteria-pocketcard/PC001. Published 2015. 7. Woolcott J, Richardson K, Wiens M, et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009;169(21):1952-1960. 8. Falls & fractures. Hyponatremia Updates website. https://www.hyponatremiaupdates.com/hyponatremia-symptoms-risks/falls-and-fractures 9. Aging & health A to Z: high blood pressure. HealthinAging.org website. http://www.healthinaging.org/aging-and-health-a-to-z/topic:high-blood-pressure/info:unique-to-older-adults/. Updated December 2017. 10. Opioid use linked to increased risk of falls, death in older adults. EurekAlert! website. https://www.eurekalert.org/pub_releases/2018-04/cmaj-oul041718.php. Published April 23, 2018. |