January/February 2017
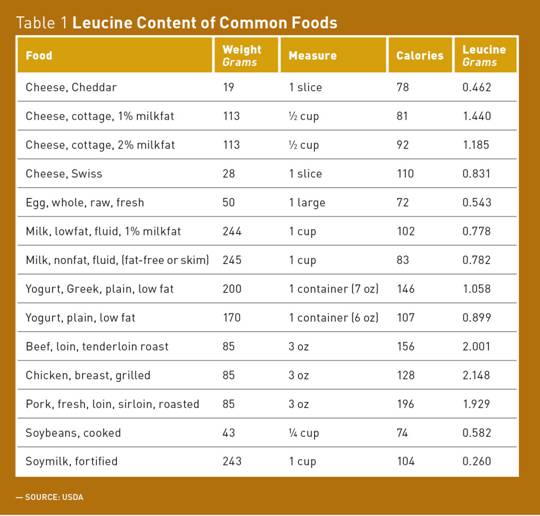
Sarcopenic Obesity — An Ominous Duo According to the Population Reference Bureau's annual report "Aging in the United States," baby boomers born between 1946 and 1964 will reshape America's older population. This year, baby boomers will be between ages 53 and 71 and the number of Americans aged 65 and older is projected to more than double from 46 million to more than 98 million by 2060. Moreover, recent estimates suggest that 37% of adults aged 65 and older are obese, a trend that is likely to increase as more baby boomers become older adults.1 During the aging process, body composition changes related to obesity and decreased muscle mass may challenge older adults' health, and the term sarcopenic obesity (SO) may unfortunately become increasingly common. High-quality protein is important for building and maintaining muscle mass. There is evidence that the source of protein may have a significant effect on helping to manage body weight and body composition. This article will discuss the ominous duo obesity and aging, the characteristics of SO, and evidence of dairy protein's role in helping to manage SO. Additionally, it will provide strategies to help older adults regain and sustain muscle strength and function. What Is SO? While there is a need for consensus on a definition for SO, it is widely recognized that the combination of obesity with sarcopenia presents an even greater risk for the elderly than either obesity or sarcopenia alone. Older adults with SO have higher risks of mobility disability, cardiometabolic diseases, and mortality.4 Nutrition Intervention for SO Muscle mass and strength start to decline as early as the age of 40.5 Researchers estimate the speed of muscle mass loss at 1% to 2% per year after the age of 50 and a decline in strength of 1.5% per year beginning at the age of 50, accelerating to 3% per year after the age of 60.6 Moreover, this natural decline in muscle mass occurs simultaneously with an increase in visceral fat and intramuscular fat.7 Weight loss in older adults, whether intentional or not, is controversial. There is evidence that being overweight may actually protect older adults against mortality and morbidity and that the harmful effects of obesity increase only at a body mass index of 30 kg/m2 or more.3 This phenomenon is known as the "obesity paradox." Additionally, weight loss is associated with a loss of muscle mass. "When anyone loses weight, you lose fat and some muscle—sometimes as much as 25% is muscle," Bales says. "Careful, slow weight loss with plenty of generous protein is recommended." Protein Quantity and Quality To help healthy older adults over the age of 65 maintain muscle mass and function, the European Society for Clinical Nutrition and Metabolism Expert Group recommends average daily intake of 1 g to 1.2 g protein per kilogram of body weight per day, and for those with SO, 1.2 g to 1.5 g protein per kilogram of body weight per day.8 Moreover, because of anabolic resistance, older adults have a higher per-meal threshold,3 and evidence shows that ~0.4 g/kg of protein per meal is needed to promote optimal MPS.9 Bales and colleagues conducted a six-month randomized controlled trial to determine whether a high protein intake (of >30 g) at each meal could protect physical function and/or lean mass during weight loss in frail obese older adults. At the six-month endpoint, there was significant (p <0.001) weight loss in both the control (−7.5±6.2 kg) and high protein (−8.7±7.4 kg) groups. Both groups also improved physical function, but the increase in the high protein (+2.4±1.7 units; p <0.001) group was greater than in the control (+0.9±1.7 units; p <0.01) group (p=0.02). The study demonstrated that a weight loss diet with enhanced meal-based protein intake was comparable to a traditional diet in achieving weight loss and superior to a traditional diet in terms of improving physical function.10 A continued debate revolves around whether the source of protein is a relevant factor. In a 2009 study published in the Journal of the American College of Nutrition, Phillips and colleagues conducted a review focusing on evidence showing the differences in responses of MPS and growth to consumption of milk and soy-based supplemental protein sources.11 The data indicate that rapidly digested whey proteins result in greater MPS than do soy proteins and that mixed milk and whey proteins are more effective than the same energy amount derived from carbohydrate. This is due, in part, to the higher leucine content of whey protein. Phillips recommends 2.5 g of leucine per meal to stimulate MPS in older adults. Other studies show that to optimally stimulate MPS in older adults, ~0.4 g/kg of leucine-rich rapidly digested protein should be consumed at each meal.9 Practical Recommendations
Yogurt, a convenient low-fat, nutrient-rich source of high-quality protein, can help older adults diversify their protein intake, especially at breakfast, where protein gaps can occur. Yogurt is a quick and easy choice that requires no cooking. Beyond protein, most yogurts contain calcium, potassium, and vitamin D, which can contribute to bone health. Adequate calcium and vitamin D as part of a well-balanced diet, along with physical activity, can reduce the risk of osteoporosis. Both bone and muscle health play key roles in maintaining a healthy, productive older population. In addition, yogurt consumption is associated with less weight gain over time, and yogurt's live and active cultures may help make it an easy dairy product to digest.14,15 The portion size of single-serve yogurt provides convenient quality protein and calorie control, and its smooth texture can be beneficial for older adults with dental issues. Summary Meal-based protein enhancement, combined with weight loss, has the potential to improve physical function in older adults with SO, reducing the risk of negative health outcomes in this high-risk population.10 — Constance Brown-Riggs, MSEd, RD, CDE, CDN, is nutrition advisor for the Dannon One Yogurt Everyday Initiative, past national spokesperson for the Academy of Nutrition and Dietetics, specializing in African American nutrition, and author of The African American Guide to Living Well With Diabetes and Eating Soulfully and Healthfully With Diabetes. References 2. Sakuma K, Yamaguchi A. Current concepts and therapeutic strategy in sarcopenic obesity. iConcept Press website. https://www.iconceptpress.com/book/obesity-epidemic/11000072/1206000746. Accessed September 17, 2016. 3. Goisser S, Kemmler W, Porzel S, et al. Sarcopenic obesity and complex interventions with nutrition and exercise in community-dwelling older persons — a narrative review. Clin Interv Aging. 2015;10:1267-1282. 4. Bouchonville MF, Villareal DT. Sarcopenic obesity — how do we treat it? Curr Opin Endocrinol Diabetes Obes. 2013;20(5):412-419. 5. Rolland Y, Czerwinski S, Abellan Van Kan G, et al. Sarcopenia: its assessment, etiology, pathogenesis, consequences and future perspectives. J Nutr Health Aging. 2008;12(7):433-450. 6. Blume SW, Curtis JR. Medical costs of osteoporosis in the elderly Medicare population. Osteoporos Int. 2011;22(6):1835-1844. 7. Stenholm S, Harris TB, Rantanen T, Visser M, Kritchevsky SB, Ferrucci L. Sarcopenic obesity — definition, cause and consequences. Curr Opin Clin Nutr Metab Care. 2008;11(6):693-700. 8. Deutz NE, Bauer JM, Barazzoni R, et al. Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN Expert Group. Clin Nutr. 2014;33(6):929-936. 9. Mazzulla M, Sawan SA, Packer JE, Moore DR. A "muscle-centric" view of dietary protein quality. Agro Food Ind Hi Tech. 2015;26(2):20-23. 10. Porter Starr KN, Pieper CF, Orenduff MC, et al. Improved function with enhanced protein intake per meal: a pilot study of weight reduction in frail, obese older adults. J Gerontol A Biol Sci Med Sci. 2016;71(10):1369-1375. 11. Phillip SM, Tang JE, Moore DR. The role of milk- and soy-based protein in support of muscle protein synthesis and muscle protein accretion in young and elderly persons. J Am Coll Nutr. 2009;28(4):343-354. 12. Chernoff R. Protein and older adults. J Am Coll Nutr. 2004;23(6 suppl):627s-630s. 13. Bernstein M, Munoz N; Academy of Nutrition and Dietetics. Position of the Academy of Nutrition and Dietetics: food and nutrition for older adults: promoting health and wellness. J Acad Nutr Diet. 2012;112(8):1255-1277. 14. Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011;364(25):2392-2404. 15. Jackson KA, Savaiano DA. Lactose maldigestion, calcium intake and osteoporosis in African-, Asian-, and Hispanic-Americans. J Am Coll Nutr. 2001;20(2 Suppl):198S-207S. |