March/April 2016
Tai Chi Intervention Reduces Fear of Falling The fear of falling in itself is a risk factor for falling. Specialized interventions can help to reduce the fear of falling and, in turn, limit the incidence of falls. The elderly population has expanded and continues to grow, representing 14.1% of the United States population in 2013, a number that is expected to increase to 21.7% by 2040, according to a 2014 US Department of Health and Human Services (HHS) estimate. Among the elderly's unique health care concerns is their increased risk for falls. Elderly adults are the population segment most likely to experience falls; each year one in three elderly adults falls, according to the Centers for Disease Control and Prevention (CDC). Falls, of course, negatively impact the elderly in various ways including physical injury, psychological distress, and death. A 2012 World Health Organization report cited falls as the second leading cause of accidental or unintentional injury deaths worldwide. According to the Emergency Nurses Association, up to one-half of older adults who are hospitalized following a fall do not survive another year. The loss of independence and the increased risk of death following a fall also lead to an increased financial burden for the nation. In 2012, falls among older adults cost the United States health care system $30 billion in direct medical costs. The CDC estimates costs will reach $54.9 billion in direct and indirect costs by the year 2020. Therefore, the health burden of falls in the elderly must be more thoroughly evaluated. Despite these daunting statistics, the CDC estimates that fewer than one-half of the elderly population have ever discussed the issue of falls with their health care providers. In a 2004 systematic review by the World Health Organization (WHO), it was suggested that prevention strategies for falls in the elderly have yet to be properly studied. Therefore it is vital to identify individuals who are at the greatest risk of falling to maximize the effectiveness of any proposed intervention. Combating Fear of Falling The purpose of a recent pilot project was to decrease the fear of falling in the elderly population residing in an assisted living facility in a rural Midwestern region through the use of a tai chi program. The assisted living facility utilized for this project had completed one fall risk assessment on residents' admission to the facility, but no further assessments related to falling were performed throughout the residents' time in the facility. Tai chi classes were offered for eight weeks in one-hour biweekly sessions. Both before and after the intervention, volunteer participants completed the Falls Efficacy Scale-International (FES-I) to determine whether changes occurred in the participants' fear of falling. The pilot project found that while a quantitative decrease in the fear of falling was not achieved, the small group of participants enjoyed tai chi classes and wanted them to continue; the majority felt the classes had exerted some impact on their balance. Fear of Falling
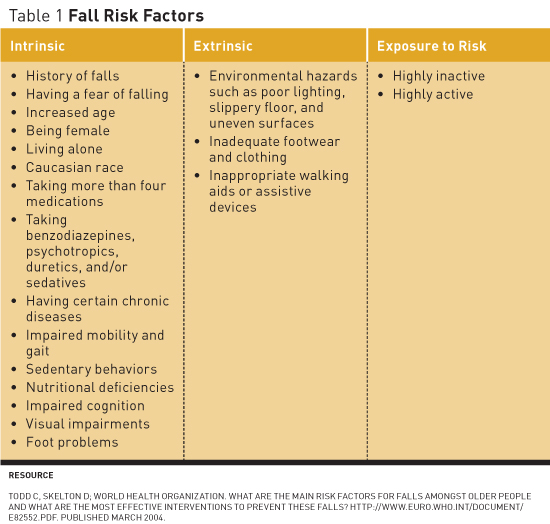
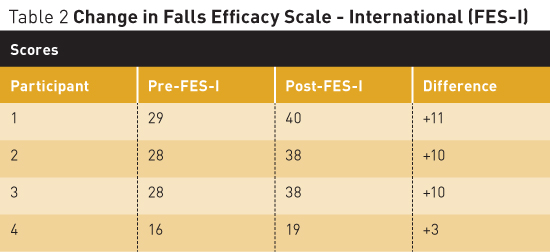
Having a fear of falling has been identified as an intrinsic risk factor for actually falling. It is defined as a lasting concern about falling that can lead to an individual's avoiding activities that he or she remains capable of performing.1 According to the American Nurses Association (ANA), an increasing body of evidence suggests that falls can cause psychological problems in many older adults, whether they have fallen in the past of have never fallen. Furthermore, the ANA notes an estimate among elderly individuals who have fallen that between 29% and 92% fear they will suffer another fall; and among those who have not fallen, between 12% and 65% fear they will fall in the future. This fear of falling causes a decrease in activity, which leads to reduced mobility and the loss of physical activity, and increases the individual's actual risk of falling, according to the CDC. Furthermore, elderly adults who develop a fear of falling limit their travel outside of their homes and their enjoyment of life experiences.2 Fear of falling was the risk factor of interest for the project described in this article. Screening for Fear of Falling Reducing the Fear of Falling In a literature review of interventions to reduce the fear of falling, it was found that six of nine studies utilizing exercise-based interventions showed a statistically significant reduction in the fear of falling.5-10 Of the three remaining studies, one demonstrated that group exercise was effective at reducing the risk factors related to falling in the elderly in an ambulatory care setting.11 Buttery et al found that 95% of the elderly were satisfied to very satisfied with participation in therapeutic exercise groups.12 Finally, McCormack et al concluded that there was no statistical significance between fear of falling and exercise interventions; however, this was a pilot study with a relatively small sample size.13 Rucker et al conducted a controlled pilot study in an emergency department aiming to reduce fear of falling in individuals aged 50 and older who had sustained a fracture postfall.14 The intervention included educational leaflets and postdischarge telephone counseling regarding fall prevention strategies. The researchers found that at three months postfall 48% of participants reported an increase in fear of falling and 11% had fallen again. Four studies were found to actually reduce falls in the elderly population through home modification interventions; however, there is limited research regarding whether they reduce the fear of falling.15-18 Tai Chi Intervention Methods and Materials The project offered tai chi classes twice per week for one-hour sessions over a period of eight weeks. The tai chi program for the elderly was developed and instructed by an American Council on Exercise-certified fitness trainer with a degree in fitness management, sports management, and health. Classes were conducted in the exercise room of the facility. Residents were provided two chairs, placed on either side, allowing them to hold on to the chairs for balance if they felt unsteady during any exercise. The fitness instructor, project leader, and activities director were present at all sessions to observe residents for any safety concerns. Prior to beginning and at the completion of the tai chi program, all participants completed the FES-I to assess their fear of falling. Results Statistical Results The FES-I scores increased after the eight weeks of tai chi (see Table 2).
The small number of participants strictly limits any statistical inference. However, this indicates that fear of falling increased postintervention. However, four qualitative questions asked at the end of the project demonstrated positive outcomes from the tai chi program. Qualitative Feedback The project leader and the tai chi instructor noted that as the classes continued, the balance and the activity of the residents appeared to improve. Increased participation with movements was noted by week three and continued throughout the remainder of the project. Likewise, by week five, the leaders noted a decrease in the need to hold on to chairs for balance. Conclusion The FES-I has been shown to have good validity, reliability, and internal structure in research studies. However, these studies were performed with elderly community-dwelling participants. The CDC places assisted living facilities collectively in the category of long term care facilities, along with nursing homes and skilled nursing facilities. Furthermore, the CDC reports that each year between one-half and three-quarters of nursing home residents fall; this is twice the rate of falls among older adults living in the community. The effectiveness of the FES-I should be specifically tested in an assisted living facility to determine whether it remains reliable and valid in this population, especially with individuals who use assistive devices for ambulation but are not completely dependent on others. The facility personnel recommended that the pre-tai chi exercise program continue with the addition of simple tai chi exercises. In addition, screening for the risk of falls and the fear of falling beyond the initial screening when residents move in to the facility to extend to an annual assessment for all residents was encouraged. A better understanding of the effect of tai chi exercises on the fear of falling would be gained with increased participation and continuation of the program for a longer period. Organizers discussed ideas to increase participation in the tai chi exercises. Suggestions included such things as reminding residents on the days of the tai chi exercises, giving recognition in the weekly newsletter to the residents for their participation, displaying pictures of participants engaged in tai chi, and offering incentives for consistent participation. Falls in the elderly present a significant health care burden. With the elderly population expected to increase to 21.7% by the year 2040, it is an issue that will continue to be a concern until the completion of further research on falls, including the development of interventions to decrease older adults' fear of falling. More research must be undertaken to examine individual risk factors for falls and to determine the effectiveness of interventions to help reduce risk factors for falls. — Abby Bennett, RN, BSN, is a DNP candidate at Creighton University in Omaha, Nebraska, with a clinical focus as a family practice nurse practitioner. — Nancy Bredenkamp, PhD, APRN, is an assistant professor of nursing at Creighton University. References 2. Emergency Nurses Association. Trauma Nursing Core Course Provider Manual. 6th ed. Des Plaines, IL: Emergency Nurses Association; 2007. 3. Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C, Todd C. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age Ageing. 2005;34(6):614-619. 4. Delbaere K, Close JC, Mikolaizak AS, Sachdev PS, Brodaty H, Lord SR. The Falls Efficacy Scale International (FES-I). A comprehensive longitudinal validation study. Age Ageing. 2010;39(2):210-216. 5. Banez C, Tully S, Amaral L, et al. Development, implementation, and evaluation of an interprofessional falls prevention program for older adults. J Am Geriatr Soc. 2008;56(8):1549-1555. 6. Brouwer BJ, Walker C, Rydahl SJ, Culham EG. Reducing fear of falling in seniors through education and activity programs: a randomized trial. J Am Geriatr Soc. 2003;51(6):829-834. 7. Dattilo J, Martire L, Gottschall J, Weybright E. A pilot study of an intervention designed to promote walking, balance, and self-efficacy in older adults with fear of falling. Educ Gerontol. 2014;40(1):26-39. 8. Gusi N, Carmelo Adsuar J, Corzo H, Del Pozo-Cruz B, Olivares PR, Parraca JA. Balance training reduces fear of falling and improves dynamic balance and isometric strength in institutionalized older people: a randomized trial. J Physiother. 2012;58(2):97-104. 9. Hill K, Womer M, Russell M, Blackberry I, McGann A. Fear of falling in older fallers presenting at emergency departments. J Adv Nurs. 2010;66(8):1769-1779. 10. Holmgren E, Gosman-Hedström G, Lindström B, Wester P. What is the benefit of a high-intensive exercise program on health-related quality of life and depression after stroke? A randomized controlled trial. Adv Physiother. 2010;12(3):125-133. 11. Rubenstein LZ, Josephson KR, Trueblood PR, et al. Effects of a group exercise program on strength, mobility, and falls among fall-prone elderly men. J Gerontol A Biol Sci Med Sci. 2000;55(6):M317-M321. 12. Buttery AK, Husk J, Lowe D, Treml J, Vasilakis N, Riglin J. Older people's experiences of therapeutic exercise as part of a falls prevention service: survey findings from England, Wales, and Northern Ireland. Age Ageing. 2014;43(3):369-374. 13. McCormack G, Lewin G, McCormack B, Helmes E, Rose E, Naumann F. Pilot study comparing the influence of different types of exercise intervention on the fear of falling in older adults. Aust J Ageing. 2004;23(3):131-135. 14. Rucker DH, Rowe B, Johnson JA, et al. Educational intervention to reduce falls and fear of falling in patients after fragility fracture: results of a controlled pilot study. Prev Med. 2006;42(4):316-319. 15. Campbell AJ, Robertson MC, La Grow SJ, et al. Randomised controlled trial of prevention of falls in people aged >=75 with severe visual impairment: the VIP trial. BMJ. 2005;331(7520):817-825. 16. Cumming RG, Thomas M, Szonyi MG, et al. Home visits by an occupational therapist for assessment and modification of environmental hazards: a randomized trial of falls prevention. J Am Geriatr Soc. 1999;47(12):1397-1402. 17. Gitlin LN, Winter L, Dennis MP, Hauck WW. Variation in response to a home intervention to support daily function by age, race, sex, and education. J Gerontol A Biol Sci Med Sci. 2008;63(7):745-750. 18. Nikolaus T, Bach M. Preventing falls in community-dwelling frail older people using a home intervention team (HIT): results from the randomized Falls-HIT trial. J Am Geriatr Soc. 2003;51(3):300-305. |