May/June 2019
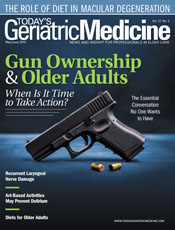
Gun Ownership and Older Adults — When Is It Time to Take Action? The Essential Conversation No One Wants to Have When an individual is diagnosed with Alzheimer’s disease, virtually every discussion becomes difficult. Questions about independence and personal autonomy that were once hypothetical become urgent and brutally relevant. Choices demand to be made, and families are forced to grapple with a future defined by a series of slow and heartbreaking goodbyes. As is the case with any catastrophic illness, this diagnosis steals the plans patients have made with their families and robs them of the future they’d always intended to share. However, once the reality of cognitive decline sets in, it becomes clear that there’s more at stake than time lost to the ravages of disease. Dementia strips away not just blocks of memories and shared history, but also some of the most familiar elements of identity and personality. As the brain becomes increasingly impaired, routines that were once committed to memory slip into disordered fragments that fall away or become impossible to retrieve. Formerly organized thinking and long-held beliefs may give way to chaos and doubt, fueled by delusion and paranoia that no reassurance can soothe. In some cases, families and the health care providers they depend upon may find themselves struggling to cope with behavior that is uncharacteristic and unpredictable. Naturally, this progression forces families to make increasingly difficult decisions. In patients with an Alzheimer’s diagnosis, reflexes will slow, perspective will become distorted and impaired, and judgment will eventually become less sound. For nearly every patient who receives an Alzheimer’s diagnosis, the day arrives when the illness warrants the significant loss of some measure of personal autonomy. Dementia, by definition, is a destroyer of order. It denies its victims any sense of control over things that, prior to diagnosis, they may have taken for granted. As the disease progresses, the patients and their families are likely to find themselves in a frightening spiral of surrendering plans and privileges, one after the other. The process is depressing and disarming, fraught with frustration for the patient and guilt for families forced to make painful choices. In many cases, it’s the loss of the ability to drive that proves to be most difficult. But for families who have a time-honored tradition of gun ownership, limiting access to firearms can be a monumental task, one that can fracture a family already strained by circumstances beyond their control. For many Americans, gun ownership is deeply rooted in family and community culture. Owning a firearm represents liberty and independence, particularly in rural America. Many gun enthusiasts see their weapons as assurance that they will never be without a means by which to protect their homes and families. It’s not especially surprising, then, that the suggestion that guns be made inaccessible, even to an individual who has been diagnosed with dementia, is likely to be met with resistance. Even under the best of circumstances, discussions about limits to gun access are delicate and emotionally charged. That complexity, compounded with the painful realities of dementia, prompts many families to put this particular conversation on a back burner and simply hope for the best. However, many families find themselves waiting for a “better time” that never actually arrives. As dementia progresses, changes in the brain prevent some individuals from understanding the extent of their cognitive limitations, and as a consequence they never see a need to alter their environments at all. Unlike denial, this condition, known as anosognosia, is a state of unawareness; it’s the inability to comprehend that an impairment exists. It’s not uncommon for caregivers to be faced with loved ones who are utterly convinced that there’s nothing wrong with their reasoning that cannot be remedied by a good night’s sleep. Attempts by family and friends to treat Alzheimer’s symptoms or to manipulate the environment for safety’s sake are viewed with suspicion and determined to be at the very least unnecessary and at the most malicious. The unfortunate truth is that by the time a family receives a diagnosis of Alzheimer’s or dementia, it may already be too late to initiate a meaningful dialogue about how to address the problem. Still, the danger of firearms in the hands of individuals with dementia is real; while the battle to preserve Second Amendment rights rages on, the fact remains that caregivers, health care providers, and concerned family members need to find an effective way to broach the subject of when it’s time to hand over the keys to the gun cabinet. A Widespread Problem While there are sufficient data to suggest that this issue at the very least warrants attention, there’s little consensus on how to best protect dementia patients, their families, and the community as a whole. From a legal standpoint, a handful of states have enacted red flag laws that permit family members and, in some cases, law enforcement, to temporarily remove firearms from individuals who have been determined by the court to be a danger to themselves or others. While these measures offer a possible solution to families with the time, resources, and wherewithal to pursue legal avenues, for many families already struggling with a catastrophic diagnosis, they are seen as a last resort. Understandably, they fear that legal action against an ill and aging loved one can do more damage than good, further fracturing a relationship already strained by grief, fear, and uncertainty. But if legal measures are not the answer, or families are not willing to make use of them, other options need to be explored that enable caregivers and health care providers to address the issue before something tragic occurs. Given the political complexities of any dialogue related to guns and gun rights, it is not surprising that many families report that no one ever suggested that firearms access should even be a consideration as related to a dementia diagnosis. However, physicians increasingly are acknowledging that they have a unique opportunity to address the issue as it relates to the health of their patients. By asking simple questions about gun access as a part of patient intake, they’re able to identify the potential for risk and address it directly in the health care setting. Following the mass shooting that occurred on October 1, 2017, in Las Vegas and left 58 people dead and another 851 injured, an article by Garen J. Wintemute, MD, MPH, was published in the Annals of Internal Medicine calling for all physicians to engage in frank discussions about firearms with their patients, addressing it as an issue related to health. Wintemute encouraged all doctors, in cases in which they see potential risk, to ask their patients about the presence of guns in the home and to follow up when it’s warranted. The suggestion has gained momentum, with many doctors pledging to include questions about access to firearms in their patient interviews. While not all physicians are fully on board with the concept of making questions about guns part of every patient’s record, some recognize that in the context of evaluating a patient diagnosed with dementia, it’s not only reasonable to do so, it’s irresponsible not to. Patients diagnosed with dementia, as well as the family members who support them, are bound to feel overwhelmed by the gravity of the diagnoses. Regardless of the extent to which they are already exhibiting symptoms of impairment, it stands to reason that initial consideration will be to their relationships, their families, and what the future may hold. It’s unlikely that in those first hours or even days following their diagnoses that they will begin making an inventory of those items in their home that may prove to be problematic. Likewise, even the most conscientious caregiver is bound to be thinking about issues that require immediate attention: treatments, care plans, and how to manage the day-to-day needs of a loved one who may not understand the extent to which their life is sure to be altered. But a caring health professional, asking the right questions in the right tone, at the right moment, can help patients and their families consider the obstacles that inevitably lie ahead. Even a thoughtfully presented list of potential dangers in the home, coupled with compassionate dialogue about the realities of disease progression, can prompt families to make important changes to the patients’ environment to help avoid calamity. When a wife understands, for example, that the time may come when her husband does not recognize their son, but views him as an unwelcome intruder, it takes no great leap to make her understand how dangerous a loaded gun could be in that equation. Likewise, by explaining that for certain patients, delusions can occur that are not only frightening but may cause them to exhibit uncharacteristic behavior, the caregivers can be made to understand that a cherished sidearm is best passed on to another family member or close friend. The Role of the Health Care Provider Naturally, not all families will respond positively. The nation is bitterly divided on issues surrounding guns and gun rights. The current political climate has increased the tension that already existed between proponents of Second Amendment rights and those who would place limits on an individual’s access to firearms. Clearly, there will be circumstances in which these discussions will be strained. For some individuals, gun ownership is an integral part of their identity, symbolic of their ability to protect the things they value most. Any suggestion that their family is somehow less safe because they have access to those guns is bound to be met with resistance. But experienced health professionals understand that there are situations that call for difficult conversations. Regardless of how the message is received, it is never an overreach to provide patients with the best information available regarding their conditions and how to manage them. In this context, for the purpose of protecting the safety of a patient and the people who provide for their care, discussion about gun access is both reasonable and prudent. In a perfect world, of course, by the time cognitive impairment becomes an issue, gun ownership would have already been addressed in the process of estate planning. With the assistance of an attorney experienced in senior law, some families have addressed the issue by creating a legally binding contract that identifies a “firearm retirement date.” Similar to an advance directive, this contract establishes a timeline, based upon chronological age or a stage of dementia, at which a trusted family member or other designee may take ownership of guns. Because the terms of the agreement are predetermined by the gun owners while they are still in full control of personal affairs, the process feels less like a surrender of rights and more like the passing down of a valued heirloom. Likewise, another option to consider is the establishment of a guns trust, an estate planning tool that’s designed to address gun ownership and legally transfer firearms to an independent trust. This apparatus simplifies the transfer of the property upon the death of the original owner and can make it easier to limit access to it when the owner becomes too impaired to use it safely. Compassionate Guidance Conversations about Second Amendment rights and guns in our communities are messy and complicated, but the question of whether a gun belongs in the hands of an individual with dementia is not. A mind impaired by the ravages of disease cannot be held accountable for a tragedy that occurs because a gun has been left unsecured and accessible. But when providers, through inaction, allow that gun to be left unsecured, without so much as a question, do they not bear some of the responsibility for that tragedy? Maybe not. But it’s better to ask, even if in asking they offend. Sometimes silence is the greater offense, the price of which can be very high. — Kathy A. Miller is a caregiver coordinator at Long Term Care Authority of Enid Area Agency on Aging in Enid, Oklahoma.
References 2. Dementia facts and statistics. Disabled World website. https://www.disabled-world.com/health/aging/dementia/statistics.php. Updated May 17, 2017. Accessed February 10, 2019. 3. Aleccia J, Bailey M. Unlocked and loaded: families confront dementia and guns. Kaiser Health News website. https://khn.org/news/dementia-and-gun-safety-when-should-aging-americans-retire-their-weapons/. Published June 25, 2018. Accessed February 10, 2019. |
