November/December 2017
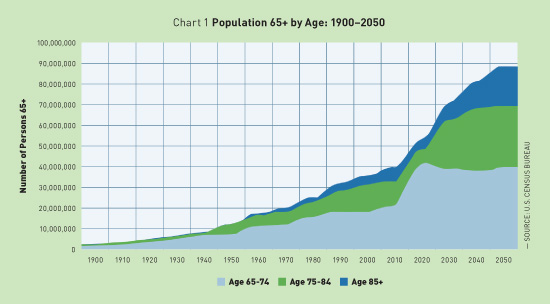
Home-Based Primary Care Transforms Health Care for Medically Complex Patients Increasing the availability of home-based primary care services offers a viable solution to the challenges of our current health care environment, increasing quality of care while significantly reducing costs in the treatment of some of our nation's costliest and neediest patients. It is no secret that the American population is rapidly aging. In fact, according to the United States Census Bureau, the number of people aged 65 and older will more than double between 2010 and 2050. By the year 2050, approximately 50 million individuals aged 75 and older are expected to be living in the United States.1 (See Chart 1.)
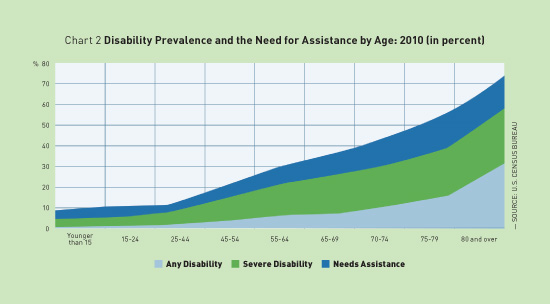
As the number of older adults grows, so too does the need for health care services. The Centers for Disease Control and Prevention reports that nearly 86% of individuals aged 65 and older have one or more chronic diseases. More than one-half of all people aged 80 and older have a severe disability, and at least 30% require assistance with activities of daily living.1 (See Chart 2.)
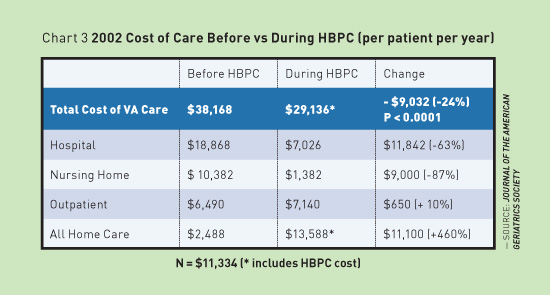
As a result, the older population represents the group with the highest levels of disability and use of costly hospital and nursing home services in the country.1-3 Unfortunately, it is this same population that has limited access to care. A Population in Need The sharp rise in older, chronically ill patients poses an increasing burden on health care providers—from physicians, nurse practitioners, and physician assistants to pharmacists and others who care for these individuals. Rising costs, lack of resources, and ever-changing policies and fee structures have left health care professionals struggling to provide cost-effective quality care for aging patients. Clearly, the current health care system is ill equipped to handle the increasing number of chronically ill patients who can't access or have difficulty accessing care outside of the home. Finding an alternative approach is necessary to care for this underserved population. Unique Approach to Care for Older Homebound Adults HBPC providers offer primary care services to these older medically complex patients whose health status, life circumstances, or a combination of both make it medically necessary to be treated in the home. Without home-based services, these patients often fail to schedule or keep appointments, are noncompliant with medications or other treatments, and rely heavily on emergency care. HBPC is different from home care services, which typically are used to help treat specific acute conditions. For example, home care may involve providing physical therapy after a fall or administering wound care for an infection. In contrast, HBPC providers care for the whole patient—the same type of care patients would receive by visiting their primary care physicians in office settings. This consistent comprehensive care can help prevent medical complications, avoid hospitalization, and allow patients to age in place. Viability of the HBPC Model For example, the VA has run an HBPC program for more than two decades, providing in-home primary care services to more than 30,000 veterans with chronic conditions. An evaluation of the program showed that in 2002, the VA's HBPC program decreased total health care-related costs by 24%, representing a cost saving of $9,000 per veteran. (See Chart 3.)
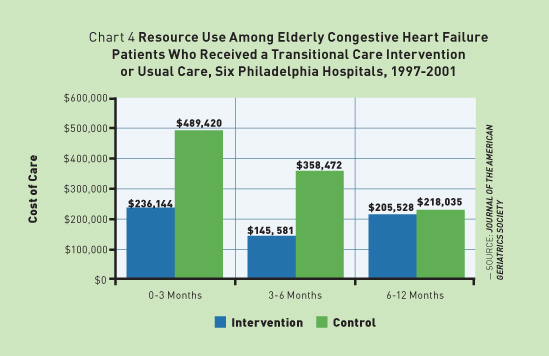
Data from 2007 showed that the program reduced hospital stays by 59%, decreased nursing home stays by 89%, and cut 30-day hospital readmissions by 21%—savings realized by HBPC services alone. The program also had the highest patient and caregiver satisfaction in the VA system.4 As an early adopter of HBPC, the VA's program illustrates the success of this model of care at both the organizational and patient levels. These statistics are mirrored by other studies on the effects of HBPC as well. For example, a 2004 study found that house calls made by nurse practitioners for three months posthospitalization cut hospital readmissions for elderly congestive heart failure patients by more than one-half. This is significant given that hospital readmission rates remain a primary concern for the health care industry. In addition, the benefits of HBPC continued beyond three months in this population but returned to baseline around six months after intervention. This demonstrates the need for ongoing in-home care.5 (See Chart 4.)
The three-year Independence at Home Demonstration Project, launched by the Centers for Medicare & Medicaid Services, also supports HBPC's ability to decrease hospital readmissions, improve patient care, and reduce overall costs. The project, which encouraged the use of home-based health care for the frailest and most costly Medicare beneficiaries, tested the ability of HBPC to reduce Medicare costs and help medically complex patients age in place. Data collected during the test support the results of other studies and illustrate the clear benefits of HBPC. In the first two years, the program realized a remarkable $32.8 million in overall savings. During these years, Independence at Home beneficiaries had fewer 30-day readmissions, hospitalizations, and emergency department visits. In addition, quality of care increased in all measured areas such as follow-up within 48 hours of hospitalization, medication reconciliation, and documented advance care preferences.6 HBPC as a Resource to Office-Based Clinicians In a sense, HBPC acts as a medical specialty. Providers can refer patients to this specialized care, ensuring the health needs of their patients are met when care in the office setting becomes difficult. Many patients receiving HBPC have chronic conditions such as congestive heart failure or end-stage renal disease that often do not significantly improve. However, for some patients, HBPC acts as a form of transitional care. If a patient becomes well enough to return to the office setting, the primary care provider can resume management of the patient's care. Unfortunately, there are currently insufficient numbers of HBPC providers to support office-based clinicians and meet the current and growing needs of this population. Although house call visits are nothing new, there have been few providers working in the field in the past decades. In fact, Medicare data from 2012 and 2013 show that there were just over 1,000 providers who performed 500 or more medical care home visits per year.7 It's not surprising then that only about 15% of the nation's home-limited patients receive primary care services in the home, leaving a vast void of needed HBPC services.8 Equipping the New Generation of HBPC Providers Opportunities within HBPC are now growing with the support of health care legislation, which recognizes the significant and growing need for primary care in the home. Portable technology now allows providers to conduct needed evaluation, testing, and treatment in remote locations, bringing expertise to the patient. In addition, the Home Centered Care Institute (HCCI), a nonprofit organization focused on advancing HBPC nationwide, has recently launched the first-ever formal training in HBPC for practitioners and business leaders. Since 2012, HCCI has worked to ensure that homebound medically complex patients have access to high-quality primary care in their homes. As part of this mission, HCCI sought to address the complete lack of training opportunities available for professionals in the field, creating a first-of-its-kind formal education training program in HBPC. HCCI Essential Elements of Home-Based Primary Care is designed to prepare health care professionals to effectively practice in the HBPC environment. The training commenced with the first group of HBPC professionals in October 2017 and is currently taking registrations from interested professionals. The First HBPC Curriculum HCCI partnered with leading academic centers and health systems throughout the country to establish the HCCI Centers of Excellence (COEs) for HBPC. These higher learning institutions serve an integral role in HCCI's education program, providing on-site classroom training for participants. HCCI's COEs include the following: • Cleveland Clinic, Essential Elements, HCCI's foundational learning experience, is made up of the following three components: Step 1: Classroom Training Step 2: Mentorship Experience Step 3: HBPC Fellowship After participants have graduated from the program, they have access to ongoing education in the field of HBPC through HCCI's extensive online learning system. This helps graduates grow their knowledge in the field and stay abreast of timely clinical and economic issues from leading experts. Advancing HBPC Nationwide Over the next five years, HCCI hopes to train 5,000 clinicians and practice managers. Our goal is to ensure that at least 50% of individuals who could benefit from HBPC have access to these services. We welcome input and involvement from professionals working in the geriatric field, those who best understand the needs of older patients. Growing HBPC within the United States health care system will have challenges. However, HCCI is working with health care leaders around the country to improve reimbursement practices, promote sustainable business models, and take steps to support, encourage, and educate professionals interested in this effective model of care. Moving HBPC into the mainstream has the potential not only to ease the industry's financial burdens and change patient lives but also to improve our health care system as a whole. To learn more about HBPC or HCCI, or to register for the foundational course, visit www.hccinstitute.org. — Thomas Cornwell, MD, is CEO of the Home Centered Care Institute in Chicago. References 2. De Jonge KE, Jamshed N, Gilden D, Kubisiak J, Bruce SR, Taler G. Effects of home-based primary care on Medicare costs in high-risk elders. J Am Geriatr Soc. 2014;62(10):1825-1831. 3. Chronic disease overview. Centers for Disease Control and Prevention website. https://www.cdc.gov/chronicdisease/overview/index.htm. Updated June 28, 2017. 4. Edes T, Kinosian B, Vukovic NH, Nichols LO, Becker MM, Hossain M. Better access, quality, and cost for clinically complex veterans with home-based primary care. J Am Geriatr Soc. 2014;62(10):1954-1961. 5. Naylor M, Brooten D, Campbell R, Maislin G, McCauley K, Schwartz J. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004;52(5):675-684. 6. Medicare Payment Advisory Commission. Report to Congress: impact of home health payment rebasing on beneficiary access to and quality of care. http://www.medpac.gov/docs/default-source/reports/december-2014-report-to-the-congress-impact-of-home-health-payment-rebasing-on-beneficiary-access-to.pdf?sfvrsn=0. Published December 2014. 7. Medicare provider utilization and payment data: physician and other supplier. Centers for Medicare & Medicaid Services website. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Charge-Data/Physician-and-Other-Supplier.html. Updated June 6, 2017. 8. Ornstein K, Leff B, Covinsky KE, et al. Epidemiology of the homebound population in the United States. JAMA Intern Med. 2015;175(7):1180-1186. |