September/October 2016
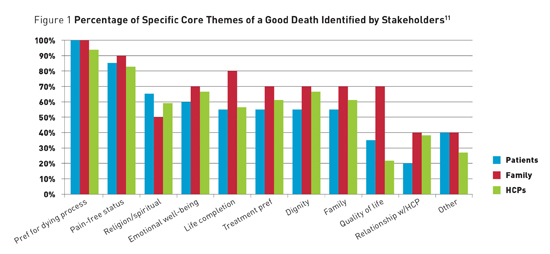
Discussing a "Good Death" With Patients Over the years, the concept of a "good death" has been considered by numerous disciplines including psychology, anthropology, sociology, and theology.1-8 Yet in recent times, death has become increasingly medicalized, with about 70% of individuals in the United States dying in hospitals, nursing homes, or long term care facilities, suggesting a need to consider what constitutes a "good death" in medical practice.9 The Institute of Medicine defines a good death as being "free from avoidable distress and suffering for patients, families, and caregivers; in general accord with patients' and families' wishes; and reasonably consistent with clinical, cultural, and ethical standards."10 The authors11 conducted a literature review examining qualitative and quantitative definitions of a "good death" and compared the perspectives of three groups of stakeholders: patients, family members, and health care providers. Thirty-six articles published between 1996 and 2015 met inclusion criteria. The sample sizes ranged from three to 2,548, and included participants ranging in age from 14 to 93, with a majority being over the age of 60. The studies had been conducted in the United States, United Kingdom, Canada, Iran, Japan, Netherlands, Thailand, and Turkey. Our review suggested 11 core themes regarding the elements of a "good death." Across the stakeholders, the three most frequent themes were preferences for the dying process (94%), pain-free status (81%), and emotional well-being (64%). Other themes included family, dignity, life completion, religiosity/spirituality, treatment preferences, quality of life, relationship with the health care provider, and other. Figure 1 shows the frequency of each of these themes,11 by stakeholder group, and illustrates both similarities and differences in the concept of a "good death," depending on whether patients, family members, or health care providers were sampled. Notably, 100% of patients noted the importance of their preferences for the dying process, highlighting the importance of end-of-life conversations in medical practice.
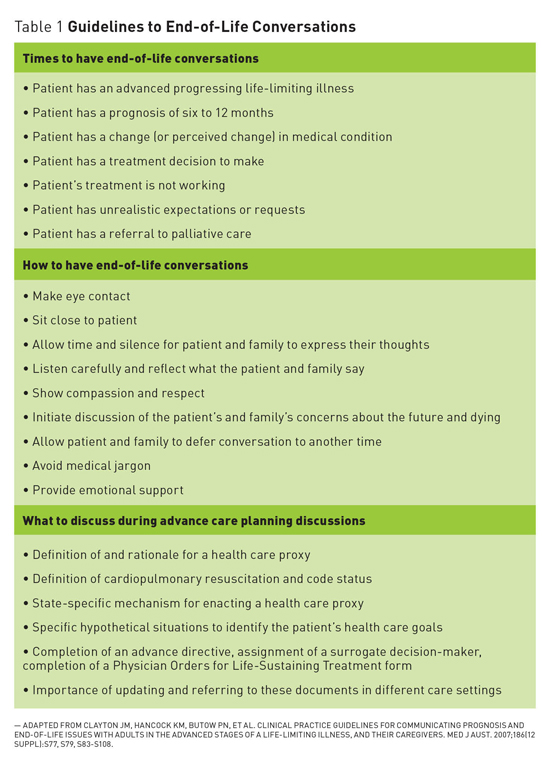
Understanding Patient Preferences When to Start the Conversation The timing and setting of such conversations are important, as patients may have difficulty processing information at the time of diagnosis, or become distressed if they do not personally initiate the conversation.14 (See Table 1.) Yet it is often challenging to decide when to start such conversations because prognostication for patients with multiple complex diseases may be unclear and there may not be a sentinel event to trigger an end-of-life conversation with the patient and the family.15
A collaborative approach, in which the provider organizes an appropriately timed family meeting to discuss the patient's progress and expectations, may be beneficial.15 Ideally, the conversations will be led by a senior member of the treatment team who can answer the patient's and family's questions.13 The optimal setting for these patient conversations and/or family meetings is a private, quiet place with plenty of time allowed for discussion and questions.13 Starting the Conversation Throughout the conversation, a physician can continually assess the patient's level of understanding with simple questions such as, "Does this make sense to you?" or "Does that seem clear?" Physicians should admit the uncertainty of prognostic predictions while reassuring patients and providing hope with statements such as: "Our team will do our best to support you throughout this illness," "I cannot give you any specific treatment to make this illness go away, but there is a lot we can offer to help you cope with it," and, "We will do everything we can to ensure you are as comfortable as possible."13 Before End-of-Life Care Go Wish Additionally, the Go Wish cards allow for individuals to further discuss and personalize specific values or goals. A professional, trainee, or family member can deliver the Go Wish intervention with minimal instruction. Case examples of using the Go Wish cards demonstrate enhanced communication and discussion of important conversations among family members as well as health care providers, helpfulness in resolving unfinished business, and assistance with surrogate end-of-life decision-making.17 POLST Challenges with POLST's implementation include having incomplete or unsigned forms, not bringing the form to different care settings, providers being unaware of the legal protections for following the POLST in certain states, providers not reading the forms, or the providers not discussing decisions with patients with intact decision-making capability or available surrogates.23 Additionally, the POLST forms do not include several interventions such as calling an ambulance, transferring patients to the emergency department or hospital, and use of all of the treatments available to hospitalized patients.21 Despite these challenges, POLST forms have been shown to improve the coordination of end-of-life care with patients' stated wishes, compared with advance directives.21 Since January 1, 2016, critical end-of-life conversations and POLST/advance directive completion are reimbursed by Medicare, allowing providers to counsel patients and families and bill appropriately for their time.24 Two new CPT codes allow physicians and nonphysician practitioners to bill for advance care planning under Medicare Part B. These changes have been supported by palliative care groups as well as an Institute of Medicine report that highlighted the critical importance of advance care planning.25-27 However, this measure should be considered as merely a first step in improving end-of-life care.28 PDQ Summary — Emily A. Meier, PhD, is an assistant professor in the department of psychiatry and a licensed psychologist specializing in end-of-life care at the University of California, San Diego Moores Cancer Center. Her clinical activities include providing both inpatient and outpatient services to cancer patients and those with advanced, life-limiting illness. Her research interests include dignity, successful dying, and training for psychologists in hospice and palliative care. — Ellen Lee, MD, is an NIH-funded research fellow in geriatric mental health at the University of California, San Diego. Her research interests include palliative care in adults with psychiatric disorders and successful aging in people with serious mental illnesses. — Lori P. Montross Thomas, PhD, is a licensed psychologist specializing in end-of-life care and a quantitative and qualitative (mixed-methods) researcher with interest in dignity, hospice care, multiculturalism, resilience, and wisdom. An assistant professor at the University of California, San Diego, she is funded by the American Cancer Society and the International Alzheimer's Association to assess positive outcomes of psychotherapy interventions for palliative care populations. — Dilip V. Jeste, MD, is senior associate dean for healthy aging, Estelle and Edgar Levi Chair in aging, and a distinguished professor of psychiatry and neurosciences at the University of California, San Diego. With research focuses on serious mental illnesses and on healthy or successful aging, he is leading both community-based and clinical studies of adults across the lifespan, examining positive traits such as resilience, optimism, and wisdom, along with biomarkers of aging. References 2. Bosek MS, Lowry E, Lindeman DA, Burck JR, Gwyther LP. Promoting a good death for persons with dementia in nursing facilities: family caregivers' perspectives. JONAS Healthc Law Ethics Regul. 2003;5(2):34-41. 3. Hart B, Sainsbury P, Short S. Whose dying? A sociological critique of the'good death'. Mortality. 1998;3(1):65-77. 4. Hattori K, Ishida DN. Ethnographic study of a good death among elderly Japanese Americans. Nurs Health Sci. 2012;14(4):488-494. 5. McNamara B. Good enough death: autonomy and choice in Australian palliative care. Soc Sci Med. 2004;58(5):929-938. 6. McNamara B, Waddell C, Colvin M. The institutionalization of the good death. Soc Sci Med. 1994;39(11):1501-1508. 7. Walter T. Historical and cultural variants on the good death. BMJ. 2003;327(7408):218-220. 8. Leichtentritt RD, Rettig KD. The good death: reaching an inductive understanding. Omega (Westport). 2000;41(3):221-248. 9. Centers for Disease Control and Prevention. Death by place, age, and race. 2005. www.cdc.gov/nchs/data/dvs/mortfinal2005_worktable_309.pdf. 10. Field MJ, Cassel CK, eds. Approaching Death: Improving Care at the End of Life. Washington, DC: National Academy Press; 1997. 11. Meier EA, Gallegos JV, Thomas LP, Depp CA, Irwin SA, Jeste DV. Defining a good death (successful dying): literature review and a call for research and public dialogue. Am J Geriatr Psychiatry. 2016;24(4):261-271. 12. Tulsky JA, Fischer GS, Rose MR, Arnold RM. Opening the black box: how do physicians communicate about advance directives? Ann Intern Med. 1998;129(6):441-449. 13. Clayton JM, Hancock KM, Butow PN, et al. Clinical practice guidelines for communicating prognosis and end-of-life issues with adults in the advanced stages of a life-limiting illness, and their caregivers. Med J Aust. 2007;186(12 Suppl):S77, S79, S83-S108. 14. Clayton JM, Butow PN, Tattersall MH. When and how to initiate discussion about prognosis and end-of-life issues with terminally ill patients. J Pain Symptom Manage. 2005;30(2):132-144. 15. Schonfeld TL, Stevens EA, Lampman MA, Lyons WL. Assessing challenges in end-of-life conversations with elderly patients with multiple morbidities. Am J Hosp Palliat Care. 2012;29(4):260-267. 16. Coda Alliance website. http://codaalliance.org. Accessed May 18, 2016. 17. Menkin ES. Go Wish: a tool for end-of-life care conversations. J Palliat Med. 2007;10(2):297-303. 18. Physician Orders for Life-Sustaining Treatment. Physician Orders for Life-Sustaining Treatment website. http://capolst.org. Updated January 1, 2016. Accessed May 11, 2016. 19. Dunn PM, Schmidt TA, Carley MM, Donius M, Weinstein MA, Dull VT. A method to communicate patient preferences about medically indicated life-sustaining treatment in the out-of-hospital setting. J Am Geriatr Soc. 1996;44(7):785-791. 20. Sabatino CP, Karp N. Improving advance illness care: The evolution of state POLST programs. AARP website. http://www.aarp.org/health/doctors-hospitals/info-04-2011/polst-04-11.html 21. Lee MA, Brummel-Smith K, Meyer J, Drew N, London MR. Physician orders for life-sustaining treatment (POLST): outcomes in a PACE program. Program of All-Inclusive Care for the Elderly. J Am Geriatr Soc. 2000;48(10):1219-1225. 22. NQF, A National Framework and Preferred Practices for Palliative and Hospice Care Quality: A Consensus Report. National Quality Forum website. http://www.qualityforum.org/publications/2006/ 23. Jesus JE, Geiderman JM, Venkat A, et al. Physician orders for life-sustaining treatment and emergency medicine: ethical considerations, legal issues, and emerging trends. Ann Emerg Med. 2014;64(2):140-144. 24. DHHS, CY 2015 Revisions to Payment Policies under the Physician Fee Schedule and Other Revisions to Medicare Part B, in CMS-1612-FC, Centers for Medicare & Medicaid Services. Published 2015. 25. NHPCO applauds new reimbursement for advance care planning conversations. National Hospice and Palliative Care Organization website. http://www.nhpco.org/press-room/press-releases/reimbursement-advance-care-planning. Published November 2, 2015. 26. Rodgers P. Medicare pay for advance care planning doesn't fall that short. American Academy of Hospice and Palliative Medicine website. http://www.aahpm.org/apps/blog/?p=2889. Published November 19, 2015. 27. Institute of Medicine of the National Academies. Dying in America: improving quality and honoring individual preferences near the end of life. http://www.nationalacademies.org/hmd/~/media/Files/Report%20Files/2014/EOL/Report%20Brief.pdf. Published September 2014. 28. Brokaw J. Medicare's move to pay doctors for end-of-life planning falls short. TIME. November 10, 2015. http://time.com/4098989/medicare-advance-care-planning/ 29. Chochinov HM, McClement S, Hack T, Thompson G, Dufault B, Harlos M. Eliciting personhood within clinical practice: effects on patients, families, and health care providers. J Pain Symptom Manage. 2015;49(6):974-980 e2. 30. Martin AS, Palmer BW, Rock D, Gelston CV, Jeste DV. Associations of self-perceived successful aging in young-old versus old-old adults. Int Psychogeriatr. 2015;27(4):601-609. |