March/April 2012
Dementia Care Model Facilitates Quality Outcomes
By Kim Warchol, OTR/L, DCCT
Aging Well
Vol. 5 No. 2 P. 32
Dementia is a broad clinical term that involves impaired mental function and memory so severe that it interferes with a person’s ability to function and live independently. Initially an individual experiences changes in activities of daily living (ADLs) such as driving, cooking, and money management. As the disease advances, he or she will have problems performing even basic ADLs such as eating, bathing, and dressing.
There have been about 100 different diseases and conditions identified that include symptoms of dementia, with Alzheimer’s disease (AD) being the most common. AD and the related dementias (ADRD) are on the rise. The latest information from the Alzheimer’s Association indicates there are currently more than 5 million people in the United States who have AD, and this number is projected to increase to between 14 and 16 million by the middle of this century.
One reason for this projected exponential rise is the fact that the No. 1 risk factor for AD is age. Currently, one of eight people aged 65 and older and almost one-half of those aged 85 and older have AD.1 Therefore, as the baby boomers age and reach their 70s and 80s, the number of people with ADRD is projected to be immense.
The prevalence of AD patients in long term care (LTC) communities is already very high and growing. Approximately 68% of nursing home residents and up to 67% of those living in assisted-living facilities have some degree of cognitive impairment related to ADRD. But about 70% of those with AD are still living at home.1 Coupling this with the fact that people with AD are three times more likely to be hospitalized than those in the same age group without AD, healthcare professionals know that many of these individuals are also using short-term rehab and home health services.
Challenges
Many studies have shown a significant correlation between the daily problems faced in LTC regarding the challenges of caring for patients with AD or dementia. AD and dementia are often identified as a root cause of common LTC problems (see Table 1 below).
To reduce these problems, it’s necessary to improve the interventions, or these challenges and poor outcomes will continue to recur.
Dementia-Capable Care
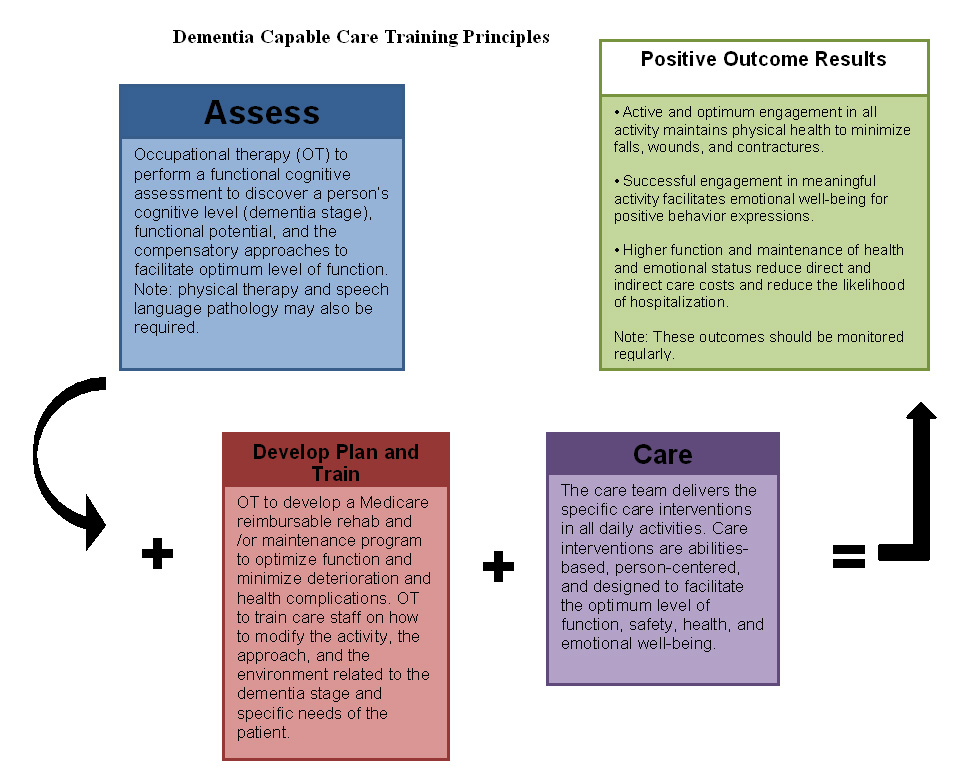
The way to create better outcomes related to serving individuals with AD or dementia is to deliver dementia-capable care. The following three components comprise the core of this innovative care model:
1. Proactive and facilitation focus: It is vital to provide care in which LTC staff “do the activity with the client to optimize function and health” rather than “doing the task for the person, which creates excess disability and health complications.” Care with the intent to facilitate active engagement and the best ability to function helps minimize the likelihood of risks such as falls, aggressive behaviors, and weight loss becoming a reality. For example, one study indicated that “when CNAs [certified nursing assistants] allow residents to control more of the eating process, they consume a higher portion of food.”2
2. Abilities-focused approach: Assessments and care interventions must focus on the person’s remaining abilities instead of what has been lost. Abilities remain at every stage of dementia, and they must be identified and capitalized on. This is a key to optimizing outcomes and the function and health of those with AD or dementia and to minimizing the care burden on staff. For example, one study said, “CNAs trained to tailor their care to the capabilities of the individual resident resulted in improvements in residents’ dressing independence.”3
3. Person-centered care: It is important to honor and integrate an individual’s life story into daily care as much as possible. This is especially important for those with AD or dementia because those individuals display better attention to activities of interest and strong long-term memory. Therefore, if LTC staff members engage the person in familiar activities, using familiar supplies associated with a familiar routine, they will facilitate higher levels of engagement, independence, and emotional well-being.
Delivering dementia-capable care requires training and ongoing commitment. The entire interdisciplinary team, including administration, direct care staff, indirect care staff, and therapists, must work together to facilitate positive outcomes. AD and dementia care is powered by specific skills and supported by leadership and an infrastructure designed to enable and encourage implementing dementia-capable care skills and techniques.
It is of utmost importance that the LTC care team realizes there is a cause and effect relationship between training, care, and outcomes, and the team must take responsibility for the outcomes. Simply stated, staff provided with effective practical dementia skills and empowered and supported to use them in daily care will create positive outcomes. Staff without training or implementation support and assistance will unknowingly create negative outcomes.
Staff must possess key skills to deliver dementia-capable care. The basic training components for all staff and leadership include the following:
• Paradigm shift: Everyone must learn what is possible for patients with AD or dementia to accomplish. Typically staff members hold low expectations, and this limits patients’ potential. It is critical to break through the negative beliefs and teach what is possible from a positive perspective. For example, “a wandering rummager” can still walk, desires to engage and explore the environment, and can use his hands to hold and move objects. These positives can be parlayed into quality outcomes instead of squelching the remaining abilities with negative labels.
• Stages: Staff must learn the functional indicators of the various dementia stages along with the key remaining abilities and the best ability to function that corresponds with each stage.
• Compensatory approaches: All staff are taught how to optimize function by compensation, which means change the environment to support and not hinder, change the approach to improve understanding and gain trust, and simplify and adapt ADLs and other activities to the appropriate challenge level.
• Communication: Staff must learn stage-specific strategies to maximize understanding between the client and the caregiver.
• Behavior management and prevention: Staff members are taught stage-specific approaches to understand the meaning behind behaviors and techniques to minimize or calm aggressive behavior, should it occur.
The dementia-capable care model relies heavily on proactive therapy intervention delivered by occupational, physical, and speech therapists with advanced education in AD and dementia evaluation and treatment. Studies support the importance and value of dementia-trained therapists, with one study that concludes, “OT [occupational therapy] has been demonstrated as effective in managing the occupational performance of people with Alzheimer’s disease.”4
There are multiple statements in the Medicare Benefit Policy Manual that support therapy services for this population. Specialized dementia therapy is needed for individuals in short-term rehab beds who have AD or dementia as a complicating factor.
Also, therapy should be offered to LTC residents with AD or dementia for the primary reason of designing a maintenance program to identify and facilitate maximum function and minimize deterioration. For therapists to deliver this type of care, they need additional education beyond the basic training outlined above. This includes the following:
• how to perform a functional cognitive assessment, such as using the Allen battery assessment tools from the Cognitive Disabilities Model by Claudia Allen, to discover cognitive level/dementia stage;
• how to utilize activity analysis and compensatory strategies to optimize function and safety at each dementia stage;
• how to design a rehab and/or maintenance program to maximize function, safety, health, and emotional well-being;
• as part of the intervention, how to educate care partners (both professional and family members) to implement the maintenance program on a daily basis; and
• how to document such skilled therapy services to receive reimbursement under Medicare Part A and B.
To facilitate positive outcomes, the dementia-capable care training principles and skills must be delivered in a supportive care model process as shown in Diagram 1 below.
Summary
We must begin using AD and dementia prevalence statistics and research studies to inform our care. ADRD aren’t going away; instead they will likely be the largest diagnostic group seen in LTC. Unmanaged or poorly managed ADRD create bad outcomes. However, there is an opportunity to create positive outcomes by empowering and supporting dementia-capable care in the workplace. This interdisciplinary, proactive care approach will enable patients living with AD or dementia to thrive, along with the people and businesses serving them.
— Kim Warchol, OTR/L, DCCT, an occupational therapist specializing in dementia management, is founder and president of Dementia Care Specialists in Hillsborough, North Carolina. Having educated more than 5,000 therapists and other healthcare professionals on an abilities-based, person-centered approach to dementia evaluation, treatment, and programming, she was instrumental in the advocacy effort that led to the 2001 Centers for Medicare & Medicaid Services’ memorandum prohibiting the denial of therapy services based solely on a dementia diagnosis.
References
1. Alzheimer’s Association, Thies W, Bleiler L. 2011 Alzheimer’s disease facts and figures. Alzheimers Dement. 2011;7(2):208-244.
2. Amella EJ. Factors influencing the proportion of food consumed by residents with dementia. J Am Geriatr Soc. 1999;47(7):879-885.
3. Beck C, Ortigara A, Mercer S, Shue V. Enabling and empowering certified nursing assistants for quality dementia care. Int J Geriatr Psychiatry. 1999;14(3):197-211.
4. Gitlin L, Corcoran M. Occupational Therapy and Dementia Care: The Home Environmental Skill-Building Program for Individuals and Families. Bethesda, MD: AOTA Press; 2005.
5. Guideline for the prevention of falls in older persons. American Geriatrics Society, British Geriatrics Society, and the American Academy of Orthopaedic Surgeons Panel on Falls Prevention. J Am Geriatr Soc. 2001;49(5):664-672.
6. Rubenstein LZ, Josephson KR, Robbins AS. Falls in the nursing home. Ann Intern Med. 1994;121:442-451.
7. Voyer P, Verreault R, Azizah M, Desrosiers J, Champoux N, Bédard A. Prevalence of physical and verbal aggressive behaviors and associated factors among older adults in long term care facilities. BMC Geriatr. 2005;5:13.
8. Zhao Y, Kuo TC, Weir S, Kramer MS, Ash AS. Healthcare costs and utilization for Medicare beneficiaries with Alzheimer’s. BMC Health Serv Res. 2008;8:108..
Table 1: Challenges Associated With Alzheimer’s/Dementia
PROBLEM |
STUDIES SHOW A CORRELATION |
Falls |
One key risk factor for falls includes many conditions associated with dementia such as cognitive impairment, impaired functioning, and depression.5
Studies show as many as three out of four nursing home residents fall each year. Falls result in disability, functional decline, and reduced quality of life.6 About 1,800 nursing home residents die each year from falls.6 |
Aggressive behavior
|
The most significant predisposing factor identified for aggressive behavior in long term care (LTC) is cognitive impairment severity. This means the more advanced the stage of dementia, the more prevalent the aggressive behavior.
Studies show 24% to 95% of LTC residents display aggressive behavior. These individuals are more likely to receive psychotropic drugs and be physically restrained. Such behaviors compromise care, can create occupational injuries among nursing staff, and can increase costs related to staff turnover and absenteeism.7 |
Costs of care |
Studies show the higher the dementia severity and/or functional dependence, the higher the direct and indirect care costs. |
Hospitalization |
Studies show people with Alzheimer’s disease and the related dementias (ADRD) are hospitalized three times more often than their peers without ADRD. AD patients are far more likely to be hospitalized for infections, pneumonia, and falls (hip fracture, syncope, collapse).8 |
(Click to enlarge.)
 | ![]()
![]()