July/August 2016
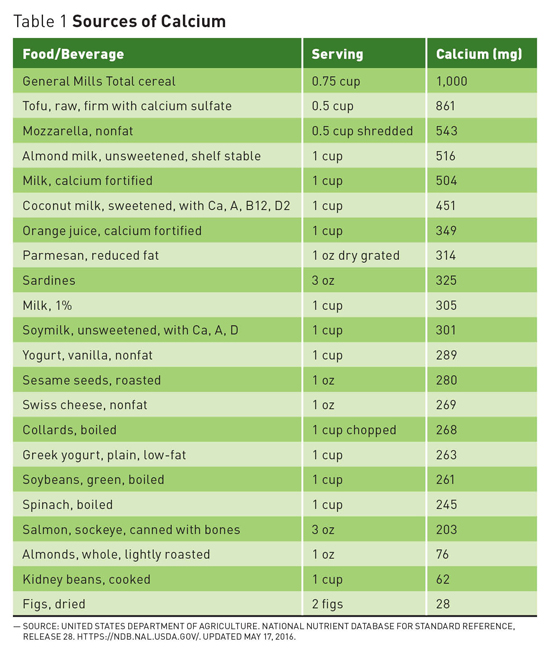
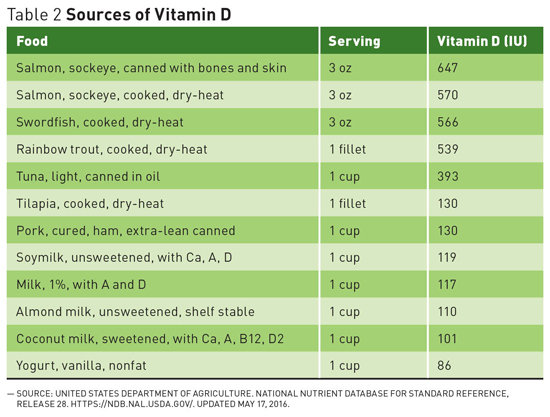
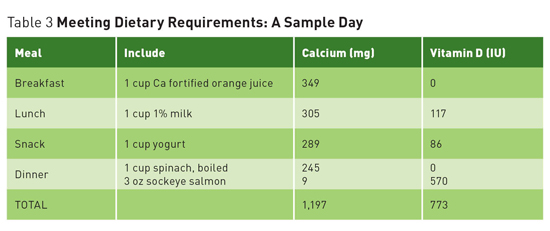
Questions on Calcium and Vitamin D Recommendations Recommended levels of calcium and vitamin D in the United States are among the highest in the world. Does research justify these levels? Are they even safe? Current studies offer conflicting results but support encouraging dietary intake over supplements. Calcium and vitamin D have long been thought to play a key role in maintaining a healthy skeleton.1 The 2011 report on dietary reference intakes for calcium and vitamin D from the Food and Nutrition Board at the Institute of Medicine (IOM) recommends that most adults aged 19 to 70 get 1,000 mg of calcium and 600 IU of vitamin D daily, with women over the age of 50 and men over the age of 70 aiming for 1,200 mg of calcium per day.1 The recommendation for 1,000 mg to 1,200 mg of calcium per day is far from universal. Britain's National Health Service recommends adults get 700 mg of calcium per day, and individuals in Nordic countries are also within the 800 mg to 900 mg range.2 A European Food Safety Authority report in May 2015 recommended 950 mg/day for adults over the age of 25.3 In 2003, the World Health Organization's report on diet, nutrition, and the prevention of chronic disease concluded that, "In countries with a high fracture incidence, a minimum of 400 mg to 500 mg of calcium intake is required to prevent osteoporosis."4 This is far below the American recommendations. Conflicting Conclusions While this study is compelling, in 2016 a meta-analysis from the National Osteoporosis Foundation reached the opposite conclusion. This analysis by Weaver et al published in Osteoporosis International showed a significant reduction in total fractures with calcium plus vitamin D supplementation, and concluded that the use of calcium plus vitamin D supplements to reduce fracture risk was supported in both community-dwelling and institutionalized older adults.6 Causes of Confusion With all of these confounding factors and variations, it may be difficult to reach a consensus. While Bolland and others believe that "there is actually no evidence of an important relationship between calcium intake and bone health in older people, and these dietary recommendations should be revised," advocacy organizations and health policymakers are standing by the IOM recommendations for now. Safety Concerns In July 2013, Reid performed a meta-analysis of randomized placebo-controlled trials of calcium supplements and found a 27% to 31% increase in the risk of heart attack and a 12% to 20% increase in the risk of stroke with calcium supplementation, with or without vitamin D.11 That same year the National Institutes of Health-AARP diet and health study suggested that high intake of supplemental calcium is associated with an excess risk of CVD death in men and recommended further research.12 But not all studies agree. "Many studies have looked carefully at the issue of calcium increasing CVD risk and are just not seeing a link," says Bess Dawson-Hughes, MD, director of the Bone Metabolism Laboratory at the Jean Mayer USDA Human Nutrition Research Center on Aging at Tufts University in Boston. A recent cohort study by Khan and colleagues, for example, found that calcium intakes of up to 1,348 mg per day from food were associated with a decreased risks of heart attack, stroke, and all-cause mortality in older men and women, as well as a decreased risk of fractures.13 According to the American Society for Bone and Mineral Research, one randomized controlled trial, one prospective cohort study, and two meta-analyses have suggested an increased risk for CVD in elderly adults on calcium supplements, and one high-quality meta-analysis, a randomized controlled trial, and several cohort studies found no evidence of such a link.14 What to Do? One area in which the data on the benefits of supplementation is unequivocal is in institutionalized elderly subjects, where calcium and vitamin D supplementation, particularly in the presence of dietary deficiencies, has been shown to reduce osteoporotic fracture risk.15 Even Bolland, who recommends against increasing calcium intake to prevent fractures in general, agrees that the evidence is conclusive in this particular population.5 For the broader population, looking for deficiency or inadequate intake is a good place to start because the positive impact of increasing intake of calcium and vitamin D is clearest in individuals who are deficient. While this issue continues to evolve, clinicians should keep a close analytical eye on emerging research and continue to encourage patients to support their bone health by quitting smoking, being physically active, and including sources of calcium and vitamin D such as dairy, fortified dairy substitutes, dark leafy greens, almonds, and beans as part of a healthful well-balanced diet. — Judith C. Thalheimer, RD, LDN, is a registered dietitian and principal of JTRD Nutrition Education Services, LLC, outside Philadelphia. References 2. Michaëlsson K. Calcium supplements do not prevent fractures. BMJ. 2015;351:h4825. 3. European Food Safety Authority Panel on Dietetic Products, Nutrition and Allergies. Scientific Opinion on Dietary Reference Values for calcium. EFSA. 2015;13(5):4101. 4. Recommendations for preventing osteoporosis. In: World Health Organization. (Diet, Nutrition and the Prevention of Chronic Diseases). Geneva, Switzerland: World Health Organization; 2003:129-131. WHO Technical Report Series 916. 5. Bolland MJ, Leung W, Tai V, et al. Calcium intake and risk of fracture: systematic review. BMJ. 2015;351:h4580. 6. Weaver CM, Alexander DD, Boushey CJ, et al. Calcium plus vitamin D supplementation and risk of fractures: an updated meta-analysis from the National Osteoporosis Foundation. Osteoporos Int. 2016;27(1):367-376. 7. Lips P, Bouillon R, van Schoor NM, et al. Reducing fracture risk with calcium and vitamin D. Clin Endocrinol (Oxf). 2010;73(3):277-285. 8. Seeman E. Evidence that calcium supplements reduce fracture risk is lacking. Clin J Am Soc Nephrol. 2010;5(Suppl 1):S3-S11. 9. Bolland MJ, Grey A, Reid IR. Should we prescribe calcium or vitamin D supplements to treat or prevent osteoporosis? Climacteric. 2015;18(Suppl 2):22-31. 10. Li K, Kaaks R, Linseisen J, Rohrmann S. Associations of dietary calcium intake and calcium supplementation with myocardial infarction and stroke risk and overall cardiovascular mortality in the Heidelberg cohort of the European Prospective Investigation into Cancer and Nutrition study (EPIC-Heidelberg). Heart. 2012;98(12):920-925. 11. Reid IR. Cardiovascular effects of calcium supplements. Nutrients. 2013;5(7):2522-2529. 12. Xiao Q, Murphy RA, Houston DK, Harris TB, Chow WH, Park Y. Dietary and supplemental calcium intake and cardiovascular disease mortality: the National Institutes of Health-AARP diet and health study. JAMA Intern Med. 2013;173(8):639-646. 13. Kahn B, Nowson CA, Daly RM, et al. Higher dietary calcium intakes are associated with reduced risks of fractures, cardiovascular events, and mortality: a prospective cohort study of older men and women. J Bone Miner Res. 2015;30(10):1758-1766. 14. Latest research on osteoporosis, bone fractures in men, calcium and vitamin D supplements and new treatments for bone disease released at ASBMR 2013 Annual Meeting. American Society for Bone and Mineral Research website. http://www.asbmr.org/About/PressReleases/Detail.aspx?cid=285ee54c-d6c1-4940-930a-4f9e87176a7c. Published October 14, 2013. 15. Boonen S, Bischoff-Ferrari HA, Cooper C, et al. Addressing the musculoskeletal components of fracture risk with calcium and vitamin D: a review of the evidence. Calcif Tissue Int. 2006;78(5):257-270.
|