July/August 2017
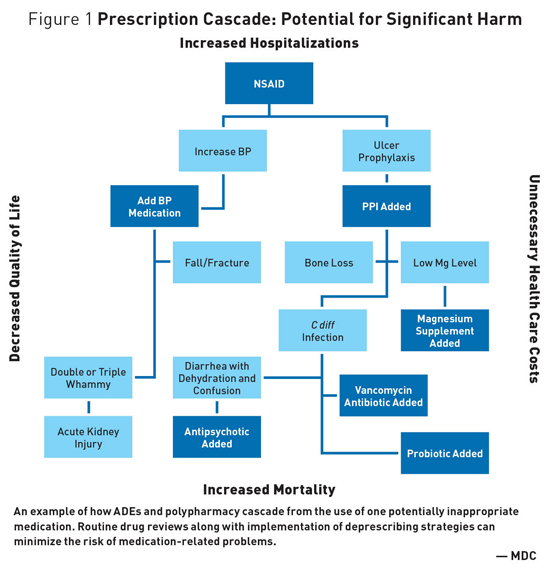
Medication Monitor: Deprescribing Improves Quality of Life Deprescribing involves reducing or stopping potentially inappropriate medications (PIMs) that may no longer be of benefit or may be causing harm. The goal is to reduce medication burden or harm while improving a patient's quality of life (QoL). Deprescribing can improve medication appropriateness by reducing polypharmacy, adverse drug events (ADEs), and other medication-related problems (MRPs).1 Evidence-based guidelines improve the treatment for a number of diseases; however, strict adherence to guidelines in frail older adults contributes to medication burden and increased MRPs.2 And while numerous guidelines exist to support prescribers in managing diseases, few guidelines provide deprescribing strategies. Prescribing requires special knowledge and close monitoring. This includes having the courage to deprescribe and the necessity of avoiding a prescribing cascade where a new medication is prescribed to "treat" side effects of another medication, while believing a new medical condition has developed. Further compounding the danger is "prescribing inertia" or the tendency to automatically renew a medication even if the original indication is no longer present. Individuals with multiple medical problems are at even greater risk for MRPs due to multiple prescribers with different specializations who focus on their own areas of expertise while no one takes an overall responsibility regarding the patient.3 Need for Routine Drug Regimen Reviews
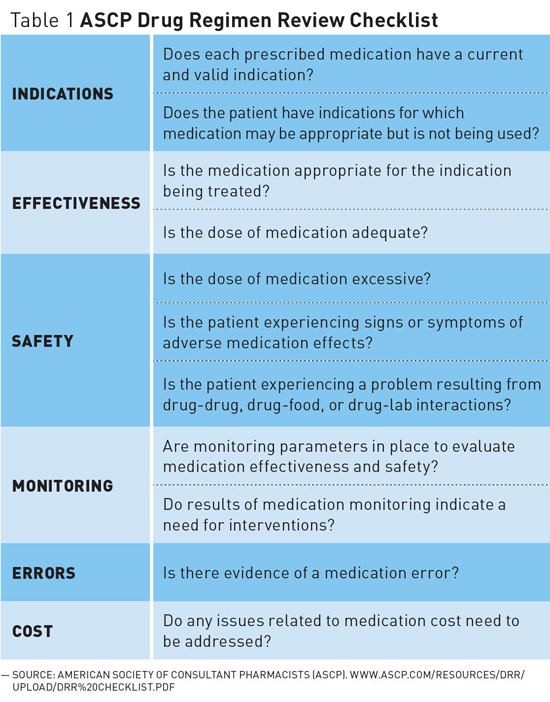
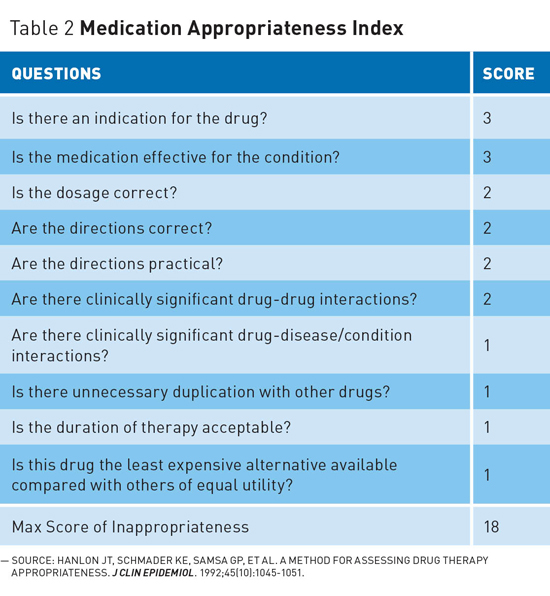
Every patient interaction should be considered an opportunity for deprescribing.4 This is especially true during transitions between care settings and has been shown to reduce MRPs. Deprescribing may require greater medication knowledge and sophistication and may be more challenging than was required to initiate drug therapy.2 For these reasons, pharmacists' role as medication experts should be maximized by prescribers and other health care team members to conduct comprehensive and often time-consuming medication reviews as well as to educate regarding efforts to improve overall deprescribing efforts. Deprescribing requires communication with patients to reach informed decisions and prioritize medications for continuation or discontinuation, in order to maximize benefit and minimize harm.2 With this mind, DRRs should individualize drug therapy based on patient preferences, life expectancy, QoL goals, comorbidities and functional status, while paying special attention to reducing pill burden, ADEs, and drug interactions.4 Medication Appropriateness Index
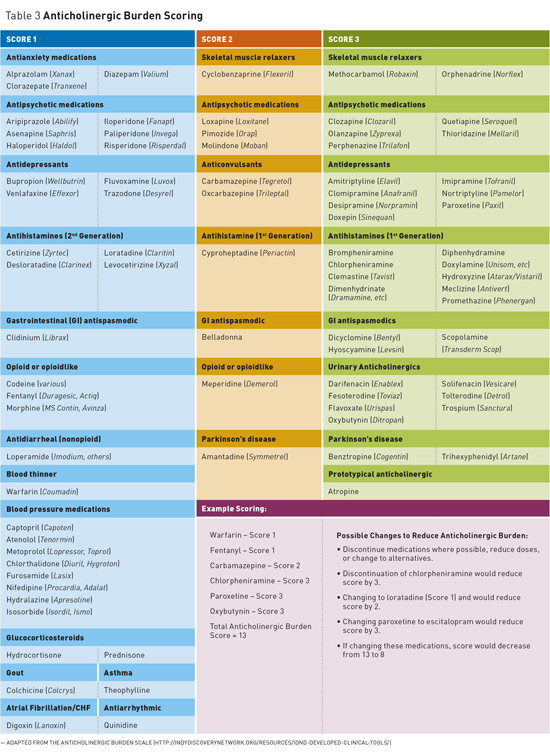
Beers Criteria • increased hospitalization when ≥2 PIMs were used together; The Beers Criteria also provide guidance on avoiding 13 combinations of medications known to cause harmful drug-drug interactions. Also noted is a specific list of 20 potentially problematic medications to avoid or that may require dosage adjustments based on kidney function.5,6 The author has been published extensively on these medications in previous editions of Medication Monitor; the Beers Criteria are accessible on the American Geriatrics Society website (www.americangeriatrics.org). STOPP Anticholinergic Burden Scales A number of scales exist to help identify meds with high anticholinergic risk while also accounting for the cumulative risk or burden. The Anticholinergic Burden Scale (ACB), for example, gives meds with possible anticholinergic effects a score of 1, while those with definite anticholinergic effects receive a score of 2 or 3 (see Table 3 for Anticholinergic Burden Scoring).8,9
Each definite anticholinergic may increase the risk of cognitive impairment by 46% over six years. A one-point increase in the ACB total score has been suggested to result in a decline in Mini-Mental State Examination score of 0.33 points over two years.8,9 In addition, each one-point increase in ACB total score has been correlated with a 26% increase in the risk of death.10 Reducing Fall Risk Medications with the greatest risk of increasing falls include anticonvulsants, antidepressants, antipsychotics, benzodiazepines (BZDs), opioids, and sedative-hypnotics. Other meds that may contribute to falls include anticholinergics, antihistamines, antihypertensives, antiarrhythmics, and skeletal muscle relaxers.5,6 Appetite Stimulants Antianxiety and Insomnia Medications BZDs are also used for anxiety and other conditions. These medications are not indicated or recommended long-term for any condition due to dependence, excessive sedation, cognitive decline, and psychomotor impairment. There is a strong correlation between BZD use and falls, which frequently result in hip and other skeletal fractures, head injury, and loss of independence. BZDs increase mortality even when use is limited to only a few doses per year, and 10% of geriatric hospitalizations have been shown to be related to the use of BZDs.13,14 Antipsychotics Some prescribers are trying Nuedexta instead; however, it is not approved for agitation or psychosis. Nuedexta has many drug interactions, may increase fall risk, and costs about $750 per month. Avoid medications for agitation or psychosis in patients with dementia.16 Instead, consider behavioral concerns such as agitation as signs of an unmet need and address with more appropriate interventions.15-18 Pain Management Proton Pump Inhibitors Steroids Diabetes Management In many older adults, higher blood glucose levels are acceptable. The American Geriatrics Society recommends A1c <8 (average glucose between 160 and 170 mg/dL) for frail older adults, those with life expectancy of less than five years, or those at risk of treatment complications. The Veterans Administration recommends A1c of <8 with life expectancy from five to 10 years and mild comorbidities while recommending hemoglobin A1c <9% with life expectancy of less than five years or major comorbidities.5 Deprescribe agents with high hypoglycemia risk, including the use of sliding scale insulin, which results in hypoglycemia without improvement in the management of hyperglycemia.5,23 Diuretic Overuse Acute Kidney Injury Lipid-Lowering Agents Nonstatins, such as niacin and fibrates, should not be used with statins, as the combination has not been shown to improve cardiovascular outcomes. Also, don't use gemfibrozil or niacin with statins due to increased risk of rhabdomyolysis and possible liver damage. Antihypertensives • Target blood pressure <150/90 for older adults over the age of 60 and especially those 80 and older. • Target blood pressure <140/90 for older adults at high risk of cardiovascular events, with diabetes or kidney disease, and doing well at lower blood pressures.
Other Medications — Mark D. Coggins, PharmD, CGP, FASCP, is vice president of pharmacy services for Diversicare, which operates skilled nursing centers in 10 states. He was nationally recognized by the Commission for Certification in Geriatric Pharmacy with the 2010 Excellence in Geriatric Pharmacy Practice Award.
References 2. Frailty, polypharmacy and deprescribing. Drug Ther Bull. 2016;54(6):69-72. 3. Olsson IN, Runnamo R, Engfeldt P. Medication quality and quality of life in the elderly, a cohort study. Health Qual Life Outcomes. 2011;9:95. 4. Frank C, Weir E. Deprescribing for older patients. CMAJ. 2014;186(18):1369-1376. 5. Coggins MD. Focus on adverse drug events. Today's Geriatr Med. 2015;8(6):8-11. 6. Pretorius RW, Gataric G, Swedlund SK, Miller JR. Reducing the risk of adverse drug events in older adults. Am Fam Physician. 2013;87(5):331-336. 7. O'Mahony D, O'Sullivan D, Byrne S, O'Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44(2):213-218. 8. Coggins MD. Antihistamine risks. Aging Well. 2013;6(2):6-7. 9. Salahudeen MS, Duffull SB, Nishtala PS. Anticholinergic burden quantified by anticholinergic risk scales and adverse outcomes in older people: a systematic review. BMC Geriatr. 2015;15:31. 10. IDND developed clinical tools: Anticholinergic burden scale. Indy Discovery Network for Dementia website. http://indydiscoverynetwork.org/resources/idnd-developed-clinical-tools/ 11. Choose wisely. American Academy of Family Physicians website. http://www.aafp.org/afp/recommendations/viewRecommendation.htm?recommendationId=183 12. Coggins MD. Unintentional weight loss and appetite stimulants. Today's Geriatr Med. 2013;6(3):10-11. 13. Coggins MD. Insomnia management. Today's Geriatr Med. 2014;7(6):6-8. 14. Coggins MD. Antianxiety medications. Today's Geriatr Med. 2017;10(2):9-11. 15. Lazare J. Reducing use of antipsychotics in nursing home patients with dementia. Today's Geriatric Medicine. January 2016. http://www.todaysgeriatricmedicine.com/enewsletter/enews_0116_01.shtml 16. Have an "exit plan" for antipsychotics in dementia patients. TRC website. https://pharmacist.therapeuticresearch.com/Content/Articles/PL/2017/Jun/Have-an-Exit-Plan-for-Antipsychotics-in-Dementia-Patients. Published June 2017. 17. Coggins MD. Behavioral expressions in dementia patients. Today's Geriatr Med. 2015;8(1):6-9. 18. Coggins MD. Dementia-related behavior management. Aging Well. 2012;5(1):32-33. 19. Coggins MD. Undertreating pain. Today's Geriatr Med. 2014;7(2):8-10. 20. Coggins MD. Tramadol safety concerns. Today's Geriatr Med. 2015;8(4):6-8. 21. Coggins MD. Recognizing proton pump inhibitor risk. Today's Geriatr Med. 2014;7(1):6-8. 22. Coggins MD. Steroid-related risks. Today's Geriatr Med. 2014;7(4):8-9. 23. Coggins MD. Sliding-scale insulin: an ineffective practice. Aging Well. 2012;5(6):8-9. 24. Coggins MD. Evaluating potential diuretic overuse. Today's Geriatr Med. 2013;6(6):5-7. 25. Coggins MD. Medication-related kidney injury. Aging Well. 2013;6(1):8-9. 26. Statin discontinuation may increase quality of life in patients with life-limiting illness. The Clinical Advisor website. http://www.clinicaladvisor.com/evidence-based-medicine/statin-discontinuation-might-increase-quality-of-life-in-patients-with-advanced-life-limiting-illness-without-affecting-median-survival/article/418522/ 27. Coggins MD. Weighing the benefits and risk of statins. Today's Geriatr Med. 2013;6(5):5-7. 28. Coggins MD. Treating hypertension. Today's Geriatr Med. 2015;8(2):6-7. |