March/April 2016
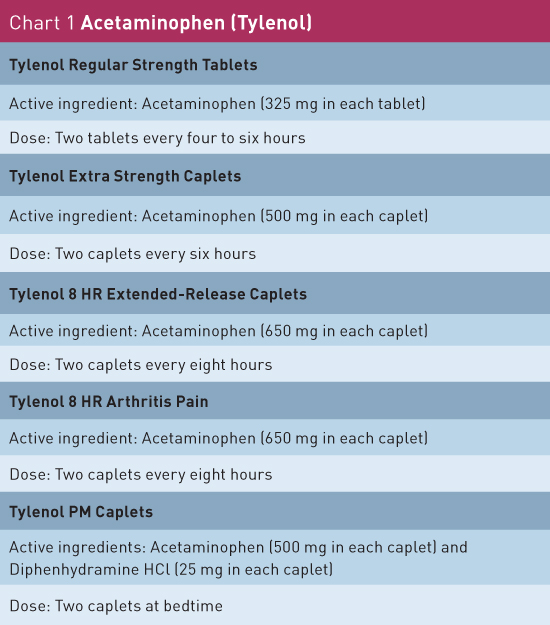
Chronic Musculoskeletal Pain: Initial Pharmacological and Nonpharmacological Therapies Concerns surrounding harmful side effects and medication interactions associated with prescription medications has led to increasing support of the use of OTC medications and nonpharmacological multimodal therapies to treat chronic musculoskeletal pain. Musculoskeletal pain is a common occurrence affecting many older adults. It is estimated that one in four older adults will suffer chronic nonmalignant musculoskeletal pain. With the increase in the geriatric population (35 million people who are aged 65 and older), the number of individuals suffering from musculoskeletal pain has grown exponentially.1 In light of this trend, it is extremely important to have a pain management strategy that helps to decrease patients' suffering and disability. The treatment options for elderly individuals can pose challenges, including concomitant medical conditions leading to drug-disease contraindications, polypharmacy with drug-drug interactions, and medical compliance with tolerance issues. Moreover, elderly individuals are high-risk candidates for surgical interventions.2 This article highlights common musculoskeletal pain conditions in the elderly and offers providers insight into the management of these conditions, utilizing nonpharmacological and over-the-counter (OTC) treatment options. Chronic Musculoskeletal Pain Conditions From 2010 through 2012, one-half (49.7%) of adults aged 65 and older reported physician-diagnosed arthritis, and it is estimated that by 2030, 67 million adult Americans could be diagnosed with the condition. According to recent statistics from the Centers for Disease Control and Prevention, nearly one in two people may develop symptomatic knee osteoarthritis by the age of 85, and one in four people may develop painful hip arthritis. In 2011, there were more than 750,000 knee and 500,000 hip replacement procedures related to arthritis alone.4-7 Chronic pain associated with arthritis can impose serious activity limitations on individuals. People can suffer significant declines in walking, climbing, bending, and social interactions; this leads to an overall decrease in quality of life. Chronic low back pain is one of the most frequently reported musculoskeletal problems. It is the third most reported symptom of any kind in individuals over the age of 75.8 A study examining Medicare data from 1991 and 2002 showed a 132% increase in the number of patients with low back pain, and a 387% increase in costs related to low back pain.9 From 1992 to 2003, the number of surgical procedures for low back pain increased significantly. For example, there was a three-fold increase in lumbar fusion surgeries in Medicare patients during that time span.10 Some potential causes of back pain in the elderly include muscle strain/sprain, compression deformities related to falls and osteoporosis, degenerative facet joint conditions, lumbar spondylosis, lumbar spinal stenosis, and lumbar disc degenerative changes. Chronic low back pain can significantly interfere with an individual's gait, mobility, and posture, and increase the risk of falls. Elderly individuals are also at high risk of fractures. Fracture sites of injury involving joints and bones not only cause acute pain conditions but can also lead to severe chronic pain conditions. It is estimated that 29% of Medicare patients living in nursing homes who have had a fracture suffer with daily chronic pain and activity limitations within six months.11 Impact of Chronic Musculoskeletal Pain Treatment Strategies Elderly individuals are at an increased risk of side effects and interactions from certain classes of prescribed medications for managing chronic pain (eg, opioids, neuromodulators, and antidepressants). Increasing evidence of this issue has led to growing support for the use of OTC medications and nonpharmacological multimodal treatment programs in older adults.12 OTC Options Acetaminophen The adult daily dose and frequency for generic acetaminophen is 325 mg to 650 mg every four hours or 650 mg to 1 g every six hours as needed for pain. The half-life of generic acetaminophen is roughly two hours; the maximum daily recommended patient-directed use, according to the FDA, is <3 g per day and, under physician-instructed use, <4 g per day. Additionally, new recommendations limit the amount of per day combination pills to 325 mg of acetaminophen.15-17 The brand name Tylenol is also available over the counter and comes with specific products for headache/muscle pain, arthritis pain, and sleep/pain (see Chart 1).
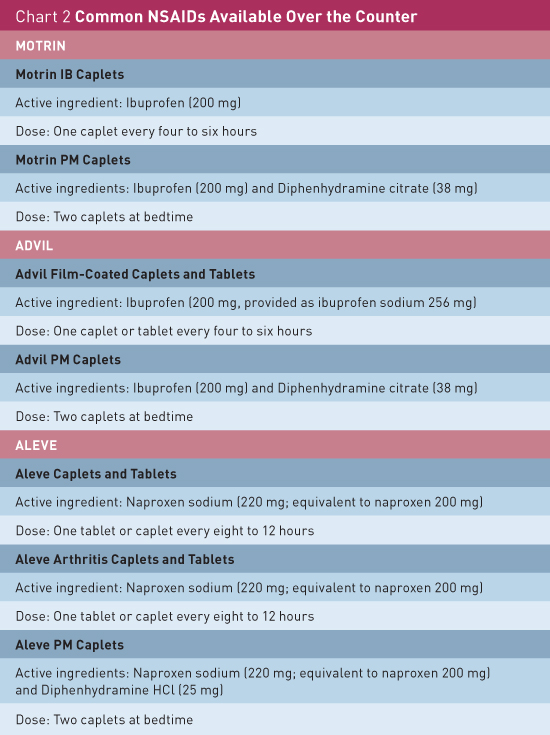
NSAIDs However, NSAIDs must be used with severe caution in older individuals due to the high risk of potentially serious and life-threatening side effects. Some of those side effects include gastrointestinal bleeding, stroke, renal failure, and ischemic heart disease. Individuals with low creatinine clearance, gastropathy, or cardiovascular disease must take NSAIDs with extreme caution due to their higher risk profile. The risk of serious complications associated with NSAIDs increases 4% for each one-year increase in age after the age of 65.18 There is also an increased likelihood of adverse gastrointestinal effects when an NSAID is coadministered with low-dose aspirin, which many elderly patients may take for antithrombotic effects. Proton pump inhibitors can help reduce the gastrointestinal effects, and the lowest effective dose should be initiated if NSAIDs are prescribed on a chronic basis.15 The following medications are NSAIDs available over the counter. Aspirin (eg, Bayer, Bufferin, and Ecotrin) is part of the salicylate family with a dosing regimen that can be prescribed at 600 mg to 1,500 mg every six hours as needed for pain. The maximum daily dosing is 2.4 g to 6 g per day with a half-life of two to three hours. Ibuprofen (eg, Motrin and Advil) is part of the propionic acid derivative family with OTC doses ranging from 200 mg to 400 mg every six hours as needed for pain. The maximum daily doses range from 1.2 g to 2.4 g for pain with a half-life of six hours. Naproxen sodium (eg, Aleve) is also part of the propionic acid derivative family. OTC doses range from 275 mg to 550 mg every 12 hours as needed for pain. The maximum daily dosing is 550 mg to 1100 mg with a half-life of 12 hours.15 (See Chart 2 for common OTC NSAIDs.)
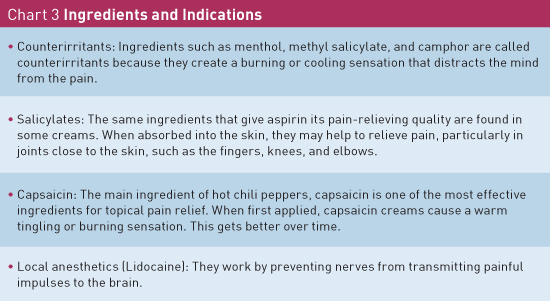
Topical Ointments
Nonpharmacologic Options Exercise Programs The most effective exercise regimen is a program that combines a patient's condition and a physical therapist. A physical therapist is responsible for planning an exercise program that generally focuses on the basic components of flexibility, strength, and aerobic education. Tai chi, a traditional Chinese mind-body exercise, has shown great promise in adults with musculoskeletal conditions and is gaining popularity. Tai chi emphasizes diaphragmatic breathing and relaxation with coordinated, smooth, gentle body movements. A 2011 study established that combined exercises (aqua/land, walking, strengthening, resistance, and tai chi) could reduce pain and disability from knee osteoarthritis. Patients suffering from other musculoskeletal conditions, such as fibromyalgia, rheumatoid arthritis, and chronic low back pain, also have reduced pain complaints with tai chi.2,21 Aquatic exercise is extremely beneficial in older adults who suffer from chronic musculoskeletal pain. The water allows for less impact on the joints with more pain-free motion. The ideal water temperature for arthritic older adults is between 85° and 90° F.2,22 Studies have shown that attendance of hydrotherapy and aquatic exercise programs is higher than that of tai chi.2,23 TENS Therapy Ice/Heat Assistive Devices Psychological Programs Interventional Targeted Treatments Conclusion — Rosemary Laird, MD, MHSA, AGSF, is a geriatrician, executive medical director of senior services for Florida Hospital at Winter Park, and past president of the Florida Geriatrics Society. She is a coauthor of Take Your Oxygen First: Protecting Your Health and Happiness While Caring for a Loved One With Memory Loss. — Ashish R. Udeshi, MD, is an interventional pain specialist with Florida Pain Institute in Merritt Island, Florida, and a board-certified anesthesiologist. He is also a voluntary assistant professor at the University of Miami in the department of clinical anesthesiology. References 2. Edeer AO, Hulya T. Management of chronic musculoskeletal pain in the elderly: dilemmas and remedies. INTECH Open Access website. http://www.intechopen.com/books/pain-in-perspective/management-of-chronic-musculoskeletal-pain-in-the-elderly-dilemmas-and-remedies. Published October 24, 2012. 3. Cooner E, Amorosi S. The Study of Pain in Older Americans. New York, NY: Louis Harris and Associates; 1997. 4. Hochberg MC, Altman RD, April KT, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken). 2012;64(4):465-474. 5. Murphy L, Schwartz TA, Helmick CG, et al. Lifetime risk of symptomatic knee osteoarthritis. Arthritis Rheum. 2008;59(9):1207-1213. 6. Barbour KE, Helmick CG, Theis KA, et al. Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation — United States, 2010–2012. MMWR Morb Mortal Wkly Rep. 2013;62(44):869-873. 7. Hootman JM, Helmick CG. Projections of US prevalence of arthritis and associated activity limitations. Arthritis Rheum. 2006;54(1):226-229. 8. Bressler HB, Keyes WJ, Rochon PA, Badley E. The prevalence of low back pain in the elderly. A systematic review of the literature. Spine (Phila Pa 1976). 1999;24(17):1813-1819. 9. Weiner DK, Kim YS, Bonino P, Wang T. Low back pain in older adults: are we utilizing healthcare resources wisely? Pain Med. 2006;7(2):143-150. 10. Weinstein JN, Lurie JD, Olson PR, Bronner KK, Fisher ES. United States' trends and regional variations in lumbar spine surgery: 1992-2003. Spine (Phila Pa 1976). 2006;31(23):2707-2714. 11. Gloth FM 3rd. Pain management in older adults: prevention and treatment. J Am Geriatr Soc. 2001;49(2):188-199. 12. Arnstein P, Herr K. Pain in the older person. In: Fishman SM, Ballantyne JC, Rathmell JP, eds. Bonica's Management of Pain. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010:782-790. 13. American Geriatrics Society Panel on the Pharmacological Management of Persistent Pain in Older Persons. Pharmacological management of persistent pain in older persons. J Am Geriatr Soc. 2009;57(8):1331-1346. 14. Udeshi AR. Pain management strategies. Today's Geriatric Medicine. 2014;7(6):14-17. 15. Buvanendran A, Lipman AG. Nonsteroidal anti-inflammatory drugs and acetaminophen. In: Fishman SM, Ballantyne JC, Rathmell JP, eds. Bonica's Management of Pain. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010:1157-1171. 16. Shega JW, Morrissey MB, Reid MC. From publication to practice: an interdisciplinary look at the labeling changes for acetaminophen and the implications for patient care. Washington, DC: Gerontological Society of America; 2011. 17. US Food and Drug Administration. Acetaminophen prescription combination drug products with more than 325 mg: FDA statement - recommendation to discontinue prescribing and dispensing. http://www.fda.gov/safety/medwatch/safetyinformation/safetyalertsforhumanmedicalproducts/ucm 18. Singh G. Recent considerations in nonsteroidal anti-inflammatory drug gastropathy. Am J Med. 1998;105(1B):31S-38S. 19. Zempsky W. Use of topical analgesics in treating neuropathic and musculoskeletal pain. Pain Medicine News. September 2013. http://painmedicinenews.com/download/TopicalsPMN070813_WM.pdf 20. Abdulla A, Adams N, Bone M, et al. Guidance on the management of pain in older people. Age Ageing. 2013;42(Suppl 1):i1-i57. 21. Ringdahl E, Pandit S. Treatment of knee osteoarthritis. Am Fam Physician. 2011;83(11):1287-1292. 22. American Geriatrics Society Panel on Exercise and Osteoarthritis. Exercise prescription for older adults with osteoarthritis pain: consensus practice recommendations. A supplement to the AGS Clinical Practice Guidelines on the management of chronic pain in older adults. J Am Geriatr Soc. 2001;49(6):808-823. 23. Fransen M, Nairn L, Winstanley J, Lam P, Edmonds J. Physical activity for osteoarthritis management: a randomized controlled clinical trial evaluating hydrotherapy or tai chi classes. Arthritis Rheum. 2007;57(3):407-414. 24. Ozyalçin NS. [Minimal invasive treatment modalities for geriatric pain management]. Agri. 2004;16(2):26-36. 25. Kloth D, Trescot A, Riegler F. Pain-Wise: A Patient's Guide to Pain Management. Hobart, NY: Hatherleigh Press; 2011. |