September/October 2020
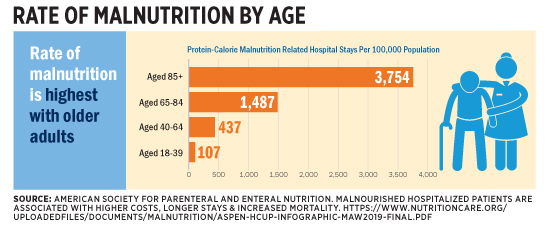
Long Term Care: Malnutrition in Older Adults With COVID-19 Infection The COVID-19 pandemic has disproportionately affected older adults. There are more than 5.3 million confirmed cases in the United States. For older adults, the rate of hospitalization is five to 13 times higher than in those aged 18–29 and the death rate is 90 to 630 times higher, according to the Centers for Disease Control and Prevention (CDC). COVID-19 is likely underreported, as many excess deaths in this population have been attributed to pneumonia.1 Hospitalized patients with COVID-19 often develop acute respiratory distress syndrome. During hospitalization, 14.2% of these hospitalized patients require ICU care and 12.2% need ventilator care.2 These patients are critically ill, hypermetabolic, and unable to eat orally. For the most part, malnutrition is a preventable and treatable condition. When untreated, it contributes to poor health and economic outcomes. Malnutrition disproportionately affects older adults. Approximately two-thirds of older adults are either at risk of becoming or are malnourished.3 Protein-calorie malnutrition–related hospital stays are five times more likely to result in death, and diagnosis rates are significantly higher in older adults (see figure). It’s also associated with longer hospital stays and higher medical costs.4
While the confirmed cases of COVID-19 continue to increase in the United States, the CDC anticipates that a second wave of disease and hospitalizations will likely occur in late 2020 through early 2021, and educating geriatrics care providers at this time is imperative. Effects of COVID-19 on Nutritional Status of Older Adults COVID-19 infection is associated with malnutrition risk, and disease-related malnutrition puts immunocompromised individuals at a higher risk of contracting this disease. These patients experience many of the following symptoms: fever, cough, shortness of breath, muscle ache, confusion, headache, sore throat, chest pain, pneumonia, diarrhea, nausea and vomiting, and loss of taste and smell, all of which may influence nutrition status and immune function.6,7 These symptoms clearly compromise nutrient intake and increase the risk for malnutrition. It’s known that older age and the presence of comorbid conditions are associated with compromised nutrition status and sarcopenia.8 With COVID-19, a high body mass index also seems to be related to poor outcomes and suggests sarcopenic obesity plays a role.9 Nutrition Screening and Assessment The majority of hospitals have implemented the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition (ASPEN) characteristics for the identification and documentation of adult malnutrition.12 This diagnostic approach includes physical assessment of muscle loss, fat loss, and the presence of edema.13 A comprehensive nutrition assessment performed by an RD is now different since the development of the COVID-19 pandemic. Many RDs are working remotely, which significantly limits physical or visual evaluation.14 Those who are working in the hospital are not entering the rooms of patients with COVID-19 infection. As a result, completion of the nutrition-focused physical exam is more difficult. RDs will use visual evaluation to note specific indentations and bony prominences to assess loss of lean and fat mass. Collaboration with primary clinicians including the bedside nursing staff and/or physician to assist with physical assessment of muscle and/or fat loss is critical to assist with identification of malnutrition in these at-risk patients. There may be greater opportunity to complete a nutrition screen in an outpatient setting than in the hospital. In the outpatient setting, nutrition screening via a validated tool is a critical step to identifying the older adult who may be at nutrition risk. Recently, the Malnutrition Screening Tool was deemed important regardless of the patient’s age, medical history, or setting.15 The Mini-Nutrition Assessment is a screening tool specifically designed and validated for the older adult and is a useful tool for the outpatient and community settings.16 Nutrition Therapy For the majority of patients with the virus who are receiving outpatient care, consider nutrition screening and assessment as outlined previously. Depending on the clinical condition of the patient, stress nutrition and hydration in their treatment. ASPEN has developed two patient education tools to help with the nutrition rehabilitation—”Nutrition and Hydration: Key Weapons in the Fight Against COVID-19” and “Nutrition and Hydration: Quick Facts for COVID-19 Patients.” Recommendations include staying hydrated; eating a high-calorie, high-protein diet; using oral nutrition supplements (if needed); and weighing yourself daily. In order to rehabilitate muscle mass, an exercise program is recommended as well. Both tools are available on ASPEN’s COVID-19 resources page at www.nutritioncare.org/COVID19. In today’s telehealth environment, education tools as outlined above—which patients can easily access, print, and review—can reinforce nutrition education and help caregivers provide these important therapeutic steps. Conclusion — Peggi Guenter, PhD, RN, FAAN, FASPEN, is senior director of clinical practice, quality, and advocacy at the American Society for Parenteral and Enteral Nutrition (ASPEN) (peggig@nutritioncare.org). — Ainsley Malone, MS, RD, LD, CNSC, FAND, FASPEN, is a clinical practice specialist at ASPEN. ASPEN is dedicated to improving patient care by advancing the science and practice of nutrition support therapy and metabolism. Founded in 1976, ASPEN is an interdisciplinary organization whose members are involved in the provision of clinical nutrition therapies, including parenteral and enteral nutrition. For more information, visit www.nutritioncare.org.
RESOURCES
MALNUTRITION AWARENESS WEEK
References 2. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052-2059. 3. Kaiser MJ, Bauer JM, Rämsch J, et al. Frequency of malnutrition in older adults: a multinational perspective using the mini nutritional assessment. J Am Geriatr Soc. 2010;58(9):1734-1738. 4. Barrett ML, Bailey MK, Owens PL. Non-maternal and non-neonatal inpatient stays in the United States involving malnutrition, 2016. U.S. Agency for Healthcare Research and Quality. https://www.hcup-us.ahrq.gov/reports/HCUPMalnutritionHospReport_083018.pdf. Published August 30, 2018. 5. The Malnutrition Quality Collaborative. National blueprint: achieving quality malnutrition care for older adults, 2020 update. https://www.defeatmalnutrition.today/sites/default/files/National_ 6. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507-513. 7. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506. 8. Graf CE, Pichard C, Herrmann FR, Sieber CC, Zekry D, Genton L. Prevalence of low muscle mass according to body mass index in older adults. Nutrition. 2017;34:124-129. 9. Peng YD, Meng K, Guan HQ, et al. Clinical characteristics and outcomes of 112 cardiovascular disease patients infected by 2019-nCoV [published online March 2, 2020]. Zhonghua Xin Xue Guan Bing Za Zhi. doi: 10.3760/cma.j.cn112148-20200220-00105. 10. Joint Commission International. Joint Commission International Accreditation Standards for Hospitals. 5th ed. Oak Brook, IL: Joint Commission Resources; 2013. 11. Patel V, Romano M, Corkins MR, et al. Nutrition screening and assessment in hospitalized patients: a survey of current practice in the United States. Nutr Clin Pract. 2014;29(4):483-490. 12. Mogensen KM, Bouma S, Haney A, et al. Hospital nutrition assessment practice 2016 survey. Nutr Clin Pract. 2018;33(5):711-717. 13. White JV, Guenter P, Jensen G, et al. Consensus statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (under-nutrition). JPEN J Parenter Enteral Nutr. 2012;36(3):275-283. 14. Mulherin DW, Walker R, Holcombe B, Guenter P; ASPEN Clinical Practice Committee. ASPEN report on nutrition support practice processes with COVID-19: the first response. https://www.nutritioncare.org/uploadedFiles/Documents/Guidelines_and_Clinical_Resources/ 15. Skipper A, Coltman A, Tomesko J, et al. Position of the Academy of Nutrition and Dietetics: malnutrition (undernutrition) screening tools for all adults. J Acad Nutr Diet. 2020;120(4):709-713. 16. Rubenstein LZ, Harker JO, Salvà A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). J Gerontol A Biol Sci Med Sci. 2001;56(6):M366-M372. 17. CDC COVID-19 Response Team. Severe outcomes among patients with coronavirus disease 2019 (COVID-19) — United States, February 12 – March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(12):343-346. 18. McClave SA, Taylor BE, Martindale RG, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr. 2016;40(2):159-211. 19. Martindale R, Patel JJ, Taylor B, Warren M, McClave SA. Nutrition therapy in the patient with COVID-19 disease requiring ICU care. https://www.nutritioncare.org/uploadedFiles/Documents/ |