September/October 2021
COVID & Nutrition — How the Pandemic Has Changed Practice The COVID-19 pandemic has had major implications in the field of nutrition. Emerging literature has outlined strategies for identifying and treating those in acute care and as they transition to outpatient settings, but there’s been limited discussion about how the pandemic has affected daily nutrition practice in postacute care, long term care, and assisted living settings, and implications for future practice.1 Malnutrition is of continued interest in geriatrics, as its prevalence increases with age and level of dependence. It has been reported to occur in as many as 29% of individuals in long term care and rehabilitation/subacute care settings, and the prevalence has been reported to be as high as 50% among all older adults.2-4 Malnutrition is characterized by nutrient imbalances; it can be a result of a number of factors, but age coupled with chronic disease, decreased taste and smell, and declines in oral, physical and cognitive function affect intake, increasing the likelihood of nutrient deficiency and resulting muscle loss.3 Acute illness compounds these challenges. Furthermore, immune function can be diminished as a result of poor nutrition status, increasing vulnerability to infection and illness.4,5 In the months since the World Health Organization declared COVID-19 a pandemic, few have felt the impact more than those in postacute care, long term care, and assisted living settings. While the long-term consequences of COVID-19 infection are still emerging, evidence indicates that symptoms affecting nutrition—including fatigue, muscle weakness, sleep difficulties, anxiety and/or depression—are persistent, suggesting that the implications of the virus will continue for some time.6 It’s been reported that more than 2 million adults reside in long term care facilities in the United States alone.7 The prevention and treatment of malnutrition in this population are influenced by complex medical and psychosocial factors including mealtime environments and quality of foods provided.4 It’s the priority of nutrition and dietetics professionals to provide individualized nutrition care and play an active role among interprofessional teams to ensure adequacy of nutrients and enhance the quality of life of residents.8 Nutrition care was significantly influenced during the first year of the COVID-19 pandemic, and there were unavoidable barriers that had to be addressed to meet the needs of this vulnerable population. This study identifies and summarizes COVID-19–related effects on nutrition practice in these settings and recognizes general trends in nutrition practice that emerged and would be beneficial to encourage in the future, with the goal of optimizing outcomes. Study approval was obtained through East Tennessee State University’s Institutional Review Board. A focus group of six registered dietitian nutritionists (RDNs) with content expertise assisted with survey development. Pilot testing and revision resulted in a 47-question, online (Qualtrics) survey, including quantitative and qualitative items related to clinical nutrition job tasks, resident feeding practices, and barriers to providing care. Twelve months after the COVID-19 pandemic was declared a public health emergency, the survey was distributed to a convenience sample of 86 RDNs and 14 certified dietary managers (CDMs) across 20 states, employed by two national companies providing services in postacute care, long term care, and assisted living settings. Participants were asked to consider their nutrition-related practice and resident outcomes over the previous 12 months. Survey response rate was 47%; 78.7% (n=37) of respondents were RDNs, and 21.2% (n=10) were CDMs; 51% held their job title for longer than 10 years. The majority of respondents described working in long term care with at least one rehabilitation unit (51.6%), long term care (28%), and assisted living (17%). The total reported number of residents served at the onset of COVID-19 was 4,616 and the mean facility census was 94.2 residents. One of the greatest challenges during the pandemic has been prioritizing individualized nutrition care for residents while managing the risks of this highly contagious virus in facilities with residents in close quarters and limited opportunities for social distancing.7-9 Additionally, while patient census numbers and budgets decreased during the pandemic, for many dietetic professionals, their job roles changed, and in some instances their responsibilities increased (25.5%). Ensuring adequate, quality nutrition is essential, but with increased infection control measures, staff illnesses, school closures, and limited recruiting opportunities for hiring, nutrition care of patients required a significant shift in procedures. One aspect affected was the ability to complete job tasks in the physical building served. While 80% of participating CDMs continued to practice in their facilities, 51.4% of RDNs were required to complete at least some of their work remotely, and 37.8% completed all work remotely. The most common tasks included completion of comprehensive nutrition assessments (51%), care plan and Minimum Data Set documentation (25.5%), and participating in high risk meetings for residents who were nutritionally compromised (21.2%). Nutrient Intake and Weight Loss Obtaining individual food preferences can improve perceived quality and intake, but with infection control requirements, it was often more challenging to get preferences (84% infection risk, 42% staffing shortage, and 42% family unable to be present). While 100% of CDMs continued to participate in this task, 15.8% of RDNs reported they assisted with obtaining food preferences more often during COVID-19 and at times communicated with residents through calls and offsite (8.5%). Prescribed nutrition interventions were also affected. Staffing (49%) and product shortages (10.1%) as well as illness-related intolerance of nutrition supplements (36%) further decreased the intake of oral nutrition supplements. Participants observed longer-term effects on appetite and resident nutrition status in residents who had COVID-19 infections within the previous 12 months. These included slow regain of appetite and sense of taste and smell, fatigue affecting self-feeding ability, and increased dysphagia and related increases in the use of mechanically altered foods. Interestingly, 76% reported increased prescriptions for mood/appetite stimulants, as well as increased perceived depression among residents. Accurate measures of weight and nutrition are key to assessing patient status, and some barriers made obtaining weights more difficult, including staffing shortages (72.3%), sanitation concerns with obtaining multiple patient weights (46.8%), and the inability to transport scales between units due to infection control concerns (61.7%). As expected, the majority of respondents (97.4%) observed moderate to significant increases in the incidence of weight loss among residents (70% significant and 27.4% moderate); 67% reported increased coding of malnutrition or at risk for malnutrition. Hydration
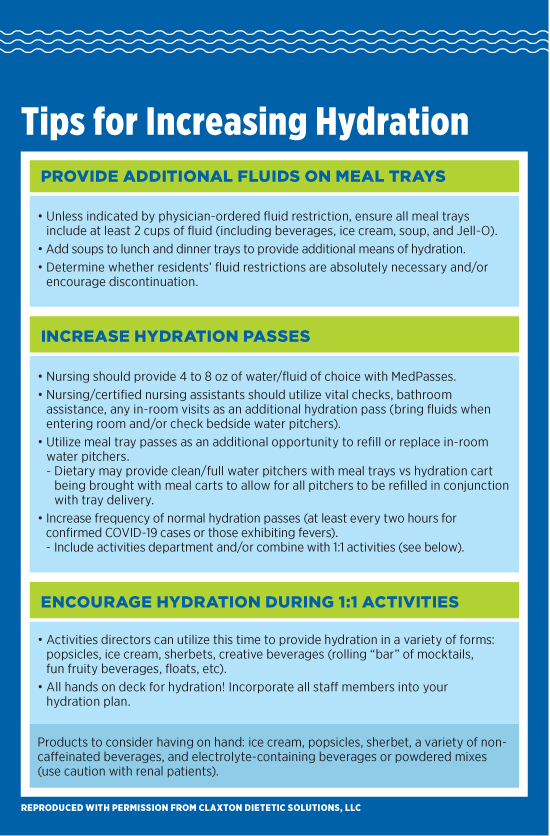
Resident Feeding Practices and Budgets Qualitative data identified similar concerns across facilities: Residents who had tested positive for the virus required disposable dishes, which cannot maintain temperatures as long as traditional service equipment and plates can. With residents required to eat in their rooms and sanitation protocols in place, meals were held longer on carts prior to delivery, causing temperature issues. Staffing shortages affected meal delivery times, with limited staffing for feeding residents efficiently in their rooms, which also influenced food temperatures. Creative delivery solutions were identified to manage proper delivery temperature, including the following: • Fewer meals were delivered on each cart to reduce service to delivery delay. Foodservice operations adjusted sanitation procedures due to increased precautions; carts required sanitizing between deliveries, and COVID-19–unit meal carts were the last to be returned for cleaning. Strengths and Opportunities Future Practice Ongoing training needs include stress management techniques, preparing for future pandemic needs, understanding how major changes affect residents’ well-being and health, ongoing teambuilding and the importance of teamwork, sanitation training for nursing and foodservice staff, the importance of hydration, and how to create a customized weighing policy. As health officials have a clearer picture of the efficacy of specific guidelines for food safety for COVID-19, newer policies can be designed as we continue to manage and recover and plan for the future.11 Best practices have been identified in the ESPEN guidelines for managing malnutrition.12 Moving forward, it will be important to focus on malnutrition risk in those previously diagnosed with COVID-19 and increase the frequency of nutrition screenings, utilizing tools such as the Mini Nutrition Assessment.2,4 This would be an efficient method of identifying ongoing risk for malnutrition alongside regularly scheduled assessments. It may also be beneficial to include COVID-specific clinical symptoms on nutrition assessment forms and in monthly high-risk patient evaluations, including diminished taste and smell, and alterations in physical and neuro-cognitive function. Understanding the role of specific nutrients in the treatment of COVID-19 and its variants will assist with the development of pandemic-specific guidelines for nutrition intake and emergency menu planning to ensure optimal outcomes for individuals.11 Additional resources can be found from the American Society for Parenteral and Enteral Nutrition on its Malnutrition Awareness Week page at nutritioncare.org/MAW. Conclusion — Michelle Johnson, PhD, RDN, LDN, is an associate professor and the director of the Dietetic Internship program in the College of Clinical and Rehabilitative Health Sciences at East Tennessee State University. She has 20 years of experience in adult and pediatric nutrition. — Julia Barroso, BS, is a graduate of Auburn University and a graduate student and dietetic intern in the clinical nutrition graduate program in the College of Clinical and Rehabilitative Health Sciences at East Tennessee State University.
References 2. Guenter P, Malone A. Long term care: malnutrition in older adults with COVID-19 infection. Today’s Geriatric Medicine. 2020;13(5):28-29. 3. Cereda E, Pedrolli C, Klersy C, et al. Nutritional status in older persons according to healthcare setting: a systematic review and meta-analysis of prevalence data using MNA®. Clin Nutr. 2016;35(6):1282-1290. 4. Volkert D, Beck AM, Cederholm T, et al. Management of malnutrition in older patients — current approaches, evidence and open questions. J Clin Med. 2019;8(7):974. 5. Butler MJ, Barrientos RM. The impact of nutrition on COVID-19 susceptibility and long-term consequences. Brain Behav Immun. 2020;87:53-54. 6. Huang C, Huang L, Wang, Y, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397(10270):220-232. 7. Gardner W, States D, Bagley N. The coronavirus and the risks to the elderly in long-term care. J Aging Soc Policy. 2020;32(4-5):310-315. 8. Dorner B, Friedrich EK. Position of the Academy of Nutrition and Dietetics: individualized nutrition approaches for older adults: long-term care, post-acute care, and other settings. J Acad Nutr Diet. 2018;118(4):724-735. 9. Bilal A, Saeed MA, Yousafzai T. Elderly care in the time of coronavirus: perceptions and experiences of care home staff in Pakistan. Int J Geriatr Psychiatry. 2020;35(12):1442-1448. 10. Picetti D, Foster S, Pangle AK, et al. Hydration health literacy in the elderly. Nutr Healthy Aging. 2017;4(3):227-237. 11. Knorr D, Khoo CH. COVID-19 and food: challenges and research needs. Front Nutr. 2020;7:598913. 12. Volkert D, Beck AM, Cederholm T, et al. ESPEN guideline on clinical nutrition and hydration in geriatrics. Clin Nutr. 2019;38(1):10-47. |