E-news ExclusiveReducing Use of Antipsychotics in Nursing Home Patients With Dementia
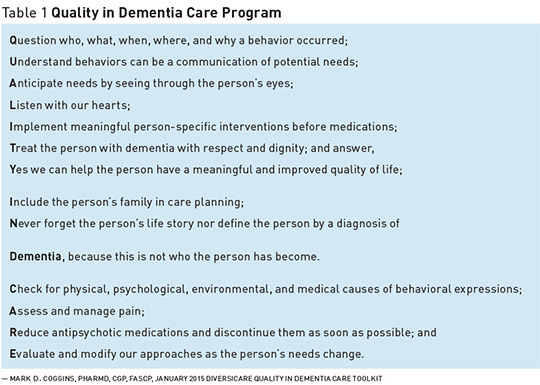
The use of antipsychotics to manage psychosis-related symptoms in elderly patients with dementia is associated with increased morbidity and mortality. Despite warnings about their harmful effects, these drugs continue to be administered. The Centers for Medicare & Medicaid Services (CMS) launched a national campaign to reduce antipsychotic use in nursing homes. Approximately one-third of elderly nursing home patients diagnosed with dementia are prescribed an antipsychotic medication to manage psychosis-related symptoms such as delusions, hallucination, aggression, and agitation.1 Antipsychotics, however, are not indicated for use in these patients and have been linked to heart failure, stroke, infection, and death. In one study, researchers used data taken from Medicaid-eligible long-stay residents in seven states and found that about 52% of residents were administered an antipsychotic without an approved CMS/FDA indication.2 The FDA requires drug manufacturers to include warning labels to alert prescribers about the increased risk of death when antipsychotics are used in patients with dementia. Despite warning labels, antipsychotic medication use in dementia patients continues in nursing homes. A report released by the Office of the Inspector General of the Department of Health and Human Services highlighted the need to reduce the use of antipsychotic medications for off-label use among nursing home residents and patients. The report revealed that 83% of nursing home residents had received an antipsychotic, but those patients had no approved diagnosis that warranted the use of antipsychotic medication.3 In 2012, CMS launched a national action plan to reduce the use of antipsychotics among older adults with dementia in long term care facilities and nursing homes. By the end of 2013, antipsychotic use across the nation had been reduced by 15%. In 2014, in an effort to underscore the importance of its campaign and reduce antipsychotic use even further, CMS established new goals to reduce antipsychotic use in nursing home residents and patients by 25% and 30% by the end of 2015 and 2016, respectively.4 One Successful Strategy Within Diversicare’s broader effort to improve quality in dementia care, there’s the desire to reduce and discontinue the potentially inappropriate use of antipsychotics for behavior management, which carries significant risk in those with dementia, says Mark D. Coggins, PharmD, CGP, FASCP, senior director of pharmacy services at Diversicare Management Services in Brentwood, Tennessee, and a director on the board of the American Society of Consultant Pharmacists. From a strategic standpoint, Coggins says that the need to obtain buy-in from leadership and staff at all levels is essential; senior leadership must get behind the initiative and work to gain support all the way to the center level. “Reducing antipsychotics is the easy part, but successful long-term antipsychotic reduction requires everyone within the center to understand best practice principles in caring for persons with dementia,” he says. “As part of our QAPI [quality assurance and performance improvement] focus, we identified a pilot center in San Antonio, which at the time had one of the highest antipsychotic rates in the company,” he says. Coggins says the plan to increase the focus on antipsychotic reduction and improved dementia care was reviewed with leadership staff at the center and was followed by staff education and training. He noted that the training included emphasizing the importance of recognizing behaviors in dementia as possibly being attempts by patients to communicate their needs; discussing the risks of using antipsychotic drugs in this population and developing individualized interventions based on a patient’s or resident’s needs and lifelong experiences; and reviewing best practice tips. “We held additional meetings with the center’s medical director, prescribers, and geriatric psychiatrist and gained support around increasing efforts to better address pain, to reduce polypharmacy, and to limit the use of antipsychotics as a last resort once all other interventions had been attempted and failed,” Coggins says. “During and following the pilot, we compiled a number of materials and best practices based on lessons learned. These materials were reviewed by multiple disciplines and incorporated into what has become our Quality in Dementia Care Toolkit (see Table 1 below), which includes tools to help reduce antipsychotic medications,” he says.
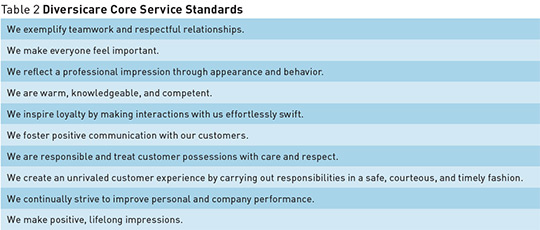
Coggins adds that Diversicare provided dementia training at its national leadership meeting held early in 2015 and engaged its leadership staff on the service standards (see Table 2 below) and how the standards should be applied not only to eliminate antipsychotic use when inappropriate, but also to manage a patient’s care in general. “The regional leadership and center leadership teams then took the lead in addressing antipsychotic use within their regions and individual centers,” he says.
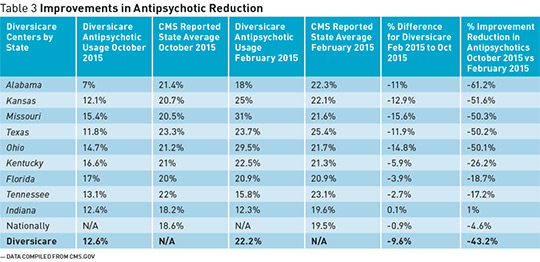
One of the most important things to aid in the effectiveness of reducing antipsychotic use was the education of staff at every level of the organization. “We created tools to be used consistently in cascading that information so that every team member was exposed to it,” says Leslie Campbell, chief operating officer at Diversicare. Through these efforts, Diversicare has been able to spearhead its progress across its facilities, even surpassing the goal set forth by CMS. Coggins says that nationally the CMS goal to reduce antipsychotic use has been very successful and should be celebrated, with about a 25% reduction over about 3 1/2 years as reported in their third quarterly report released in 2015. “We experienced about a 10% reduction within the first month, 30% by the fourth month, and we currently have reduced [antipsychotic] use by 56.25% going from 22.4% in February 2015 to 12.6% in October 2015,” he says. Diversicare operates 55 nursing care facilities in nine states. Table 3 below compares the improvements in the reduction of antipsychotic use in each of these states as reported by Diversicare and CMS. Coggins adds that Diversicare’s success lies in discussing patients and their needs during daily clinical start-up meetings. When patients’ behaviors change, the health care team conducts multidisciplinary meetings to evaluate what potential needs may need to be addressed, to assess the nonmedication interventions that have been tried, to determine what other interventions can be implemented, and to consider whether the behavior truly warrants the use of an antipsychotic, while weighing the risks and benefits.
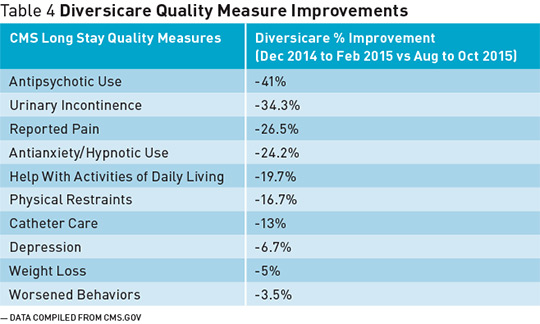
Staff Training Improves Quality Measures Campbell also points out that when staff fails to recognize that dementia compromises the ability to communicate fluently and that certain behaviors are reflective of patients’ unmet needs or desires, an antipsychotic may be inappropriately given to manage these patients. So changing the way that team members think about these behaviors reduces the introduction of an antipsychotic medication. “Our frontline caregivers take a great deal of pride and personal satisfaction and gratification in preventing these episodes of behaviors and then preventing the introduction of an antipsychotic medication,” she says. Diversicare’s efforts, Coggins says, have been based around educating staff about what they need to assess in patients with dementia and ensuring that leadership is on board in understanding that antipsychotic medications are not be used unless they’re absolutely necessary. The antipsychotic is not going to be effective, for example, if the reason a patient is behaving in a disruptive manner is associated with pain. So it’s essential to evaluate the physical, psychological, environmental, and medical causes of such behaviors rather than first giving a drug. If pain is identified as the cause of the behavior, treat the patient appropriately for pain, which may remove the cause of the behavior, he says. Through proper staff training, Diversicare has been able to reduce antipsychotic use and improve quality measures at its nursing care facilities nationwide. Table 4 below shows its improvements related to CMS-specific long-stay quality measures such as urinary incontinence, depression, and worsening behavior. Campbell says, “Along with the reduction in the overall use of antipsychotics in our patient and resident population, we saw a very significant improvement in our quality measure outcomes.”
In reviewing our data, there appears to be a strong correlation between the reduction of antipsychotic medication and the improvement of key quality measures,” Campbell says. Diversicare’s program also led to improved pain management, reduced depression and anxiety, reduced prevalence of urinary incontinence, and decreased use of anxiolytics and hypnotics, she says. “All of those reductions were accomplished absent an increase in physical restraints or falls. We're really proud of the overall improvement in quality measures.” The shift in reducing antipsychotic use and negative outcomes is associated with staff training. “Central to the effort was the way we set out to change the way we talked about these patients or residents and modified the way we referenced behaviors,” Campbell says. Approaches to Reducing Antipsychotic Use • Involve the entire medical staff. It’s integral that an organization’s medical director and other leadership staff understand the materials from quality improvement organizations and CMS on the use of antipsychotics, according to Gail Geisenhoff, vice president of clinical services at Diversicare. Educating staff at all levels helps to identify organizational behaviors, improve interdisciplinary communication, and achieve better prescribing practices in nursing homes.5 • Identify nonpharmacological interventions. “First look at your PRN [medications administered on an as-needed basis],” Geisenhoff says. “We shouldn’t be giving antipsychotics as a PRN because that really isn’t how they’re meant to [be used]. There are nonpharmacological interventions that need to be used before any medication with expressions of unmet needs or behaviors.” With the support from the Commonwealth Fund and the John A. Hartford Foundation, a free online toolkit that provides nonpharmacological approaches is available to assist nursing home staff in addressing neuropsychiatric symptoms in dementia patients. • Track and review antipsychotic use. “We receive a flag when someone is admitted to one of our facilities on an [antipsychotic] medication. We also tracked and trended physicians’ prescribing practices, which was helpful to us in identifying areas of opportunity where we could better partner with our prescribers,” Campbell says. Geisenhoff notes that tools are necessary to help all team members at a center recognize that the answer isn’t necessarily always a medication. Staff members need to take the time to understand why patients may behave in a certain way and respond to specific issues and develop a basic understanding of antipsychotics and how dangerous they are in patients with dementia. • Promote success through visibility. Geisenhoff says that daily visibility of the actual numbers in real time with electronic physician orders and sharing success stories are components that help to reduce antipsychotic use. “The visibility to the numbers and the percentages compared to the national and state averages are important to look at all the time, and most people could pull that [information] pretty easily from their electronic physician orders. When you start benchmarking and showing what others can do, and then you hear those individual stories of success, I think it’s motivating,” Geisenhoff says. • Increase the presence of all health care professionals. Campbell points out that it’s important to increase the presence of practitioners, particularly physician extenders. “We’re in the process of implementing an in-house nurse practitioner model in several of our markets.” She also notes that organizations must include the consulting pharmacist as an integral member of the care teams and recognize the value the consultant pharmacist brings to interdisciplinary teams. Pharmacists have such a deep expertise in and knowledge of medications, which can help reduce negative medication-related outcomes, including adverse drug events, as well as helping us continue to improve the care for residents and patients, she says. Coggins agrees that centers need to increase the visibility of the consultant pharmacist as the expert on medication management because he or she plays an important role in managing prescribing habits on an ongoing basis in nursing homes. If the pharmacist notes that the medications being used are likely not the most appropriate, then quality assurance efforts should focus on working with the pharmacist and other members of the interdisciplinary team to have candid conversations about what needs to be done to ensure medication use is appropriate, effective, and safe. • Engage the family members. “We need to involve the family in care planning, so the staff can understand what has bothered a patient at home. A patient’s family may inform staff that when there are many people around him or her, he or she becomes agitated, nervous, and anxious. Staff can include this information in the patient’s care plan to keep him or her in a quiet environment,” Coggins says. “Medication management is complex, and I am not under the belief that any one prescriber, pharmacist, nurse, or any other individual can achieve better outcomes than that of a well-functioning team represented by multiple disciplines,” Coggins says. — Jaimie Lazare is a freelance writer based in Brooklyn, New York.
References 2. Lucas JA, Chakravarty S, Bowblis JR, et al. Antipsychotic medication use in nursing homes: a proposed measure of quality. Int J Geriatr Psychiatry. 2014;29(10):1049-1061. 3. Centers for Medicare & Medicaid Services. Interim report on the CMS National Partnership to Improve Dementia Care in Nursing Homes: Q4 2011 — Q1 2014. https://www.cms.gov/medicare/provider-enrollment-and-certification/surveycertificationgeninfo/downloads/survey-and-cert-letter-14-19.pdf. Published April 11, 2014. Accessed December 19, 2015. 4. National Partnership to Improve Dementia Care in Nursing Homes. Centers for Medicare & Medicaid Services website. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/National-Partnership-to-Improve-Dementia-Care-in-Nursing-Homes.html. Updated December 2, 2015. Accessed December 19, 2015. 5. Tjia J, Gurwitz JH, Briesacher BA. The challenge of changing nursing home prescribing culture. Am J Geriatr Pharmacother. 2012;10(1):37-46. |